Stem cells are sometimes seen as either controversial or lifesaving, depending on what they are being used for, but a new breakthrough in the treatment of multiple sclerosis (MS) has researchers and patients alike looking at the technology in a different way. Using the same approach as some forms of chemotherapy, along with autologous haematopoietic stem cell transplantation (aHSCT) researchers have shown that 23 out of 24 patients have experienced a full on halt of clinical relapses as well as the absence of new brain lesions of multiple sclerosis for a prolonged period without the need for ongoing medication.

Results published recently in The Lancet show that a phase 2 clinical trial of this new therapy resulted in unprecedented improvement for some patients Eight of 23 study particpants showed a sustained improvement in their disability 7.5 years after treatment. While these results are cause for celebration, treatment related risks are still a factor and scientists caution that the use of this new therapy is not likely to be widespread just yet.
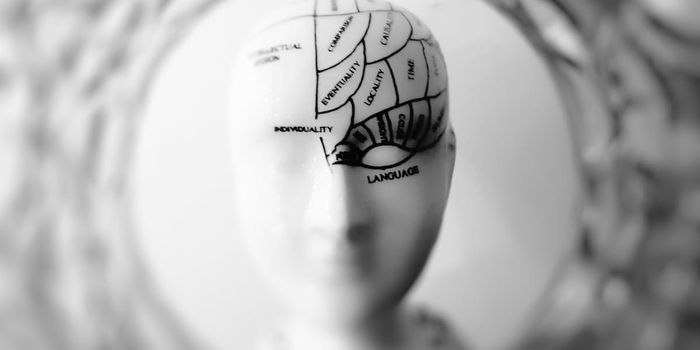
MS affects about 2 million people worldwide. Inflammation caused when the body’s own immune system attacks the central nervous system can wreak havoc with cognitive functions, muscle movement, and motor impairment. While the process of harvesting bone marrow to get stem cells and then shutting down the immune system with chemotherapy is a novel and new approach to reset the body’s autoimmune response, not every patient responds well to this treatment
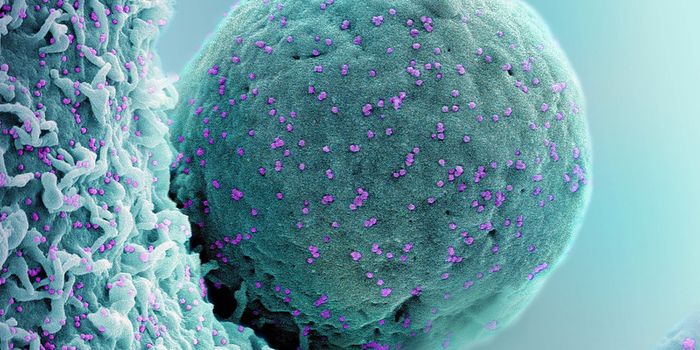
While suppressing the immune system has been the norm, the new research has taken it a step further. Dr Harold L Atkins and Dr Mark S Freedman from The Ottawa Hospital and the University of Ottawa, Ottawa, Canada tested whether completely wiping out a patient’s immune system, rather than just suppressing it during aHSCT would reduce the relapse rate in patients and increase long-term disease remission.
They enrolled 24 patients aged 18-50 from three Canadian hospitals who had all previously undergone the standard protocol of immunosuppressive therapy but had not experiences complete control of their MS symptoms. All of the patients in the study had poor prognoses and their disability ranged from moderate to requiring a walking aid to walk 100m according to standard evaluations of disabilities.
The researchers used a similar method of aHSCT as is currently used, but instead of just suppressing the immune system before transplantation, they destroyed it completely using a chemotherapy regimen of busulfan, cyclophosphamide and rabbit anti-thymocyte globulin. In a press release, Dr Atkins explains that this treatment is "similar to that used in other trials, except our protocol uses stronger chemotherapy and removes immune cells from the stem cell graft product. The chemotherapy we use is very effective at crossing the blood-brain barrier and this could help eliminate the damaging immune cells from the central nervous system."
The study resulted in 23 of the 24 patients experiencing multiple sclerosis activity-free survival at 3 years (as measured by relapses of MS symptoms, new brain lesions, and sustained progression of EDSS scores). Sadly, one patient in the study died from hepatic necrosis and sepsis caused by the chemotherapy. Prior to the treatment, patients experienced 1.2 relapses per year on average. After the grueling regimen of chemo, no relapses occurred during the follow up period in the surviving 23 patients These clinical outcomes were confirmed by MRI scans as well. The initial 24 MRI scans revealed 93 brain lesions, and after the treatment only one of the 327 scans showed a new lesion
Dr Freedman, the co-author of the paper advised caution despite the hopeful results, stating, "The sample size of 24 patients is very small, and no control group was used for comparison with the treatment group. Larger clinical trials will be important to confirm these results. Since this is an aggressive treatment, the potential benefits should be weighed against the risks of serious complications associated with aHSCT, and this treatment should only be offered in specialist centres experienced both in multiple sclerosis treatment and stem cell therapy, or as part of a clinical trial. Future research will be directed at reducing the risks of this treatment as well as understanding which patients would best benefit from the treatment.” Check out the video below for more information
Sources:
The Lancet,
Multiple Sclerosis Trust,
Ottowa Hospital/University of Ottowa