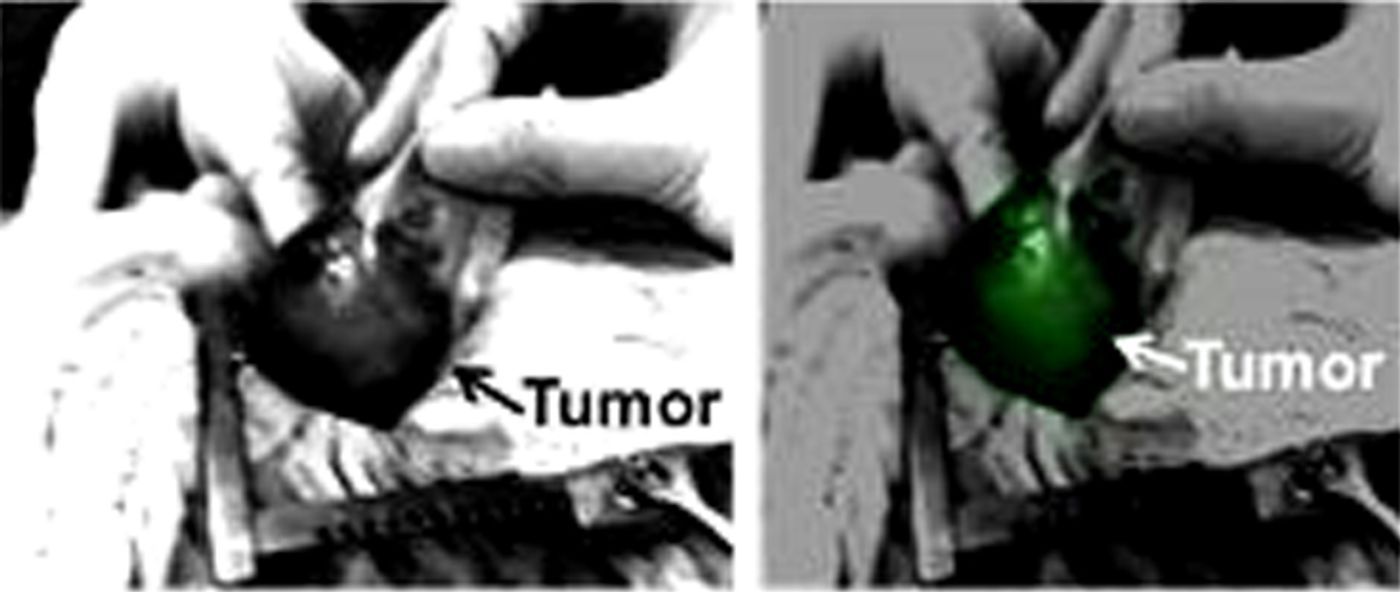
In as much as 50 percent of operations to remove brain tumors, some cancerous bits are left behind and the cancer makes a most unwelcomed return. Now, researchers at the University of Pennsylvania say a t
echnique that makes brain tumors fluoresce during surgery will enable more thorough removal and minimize tumor recurrence.
Each year, surgeons operate on over 15,000 patients to remove brain tumors. The extremely delicate nature of these operations already put patients at increased risks for complications. Furthermore, the success of the operation is drastically minimized when tumor tissues are left behind because the tumor margins are difficult to identify.
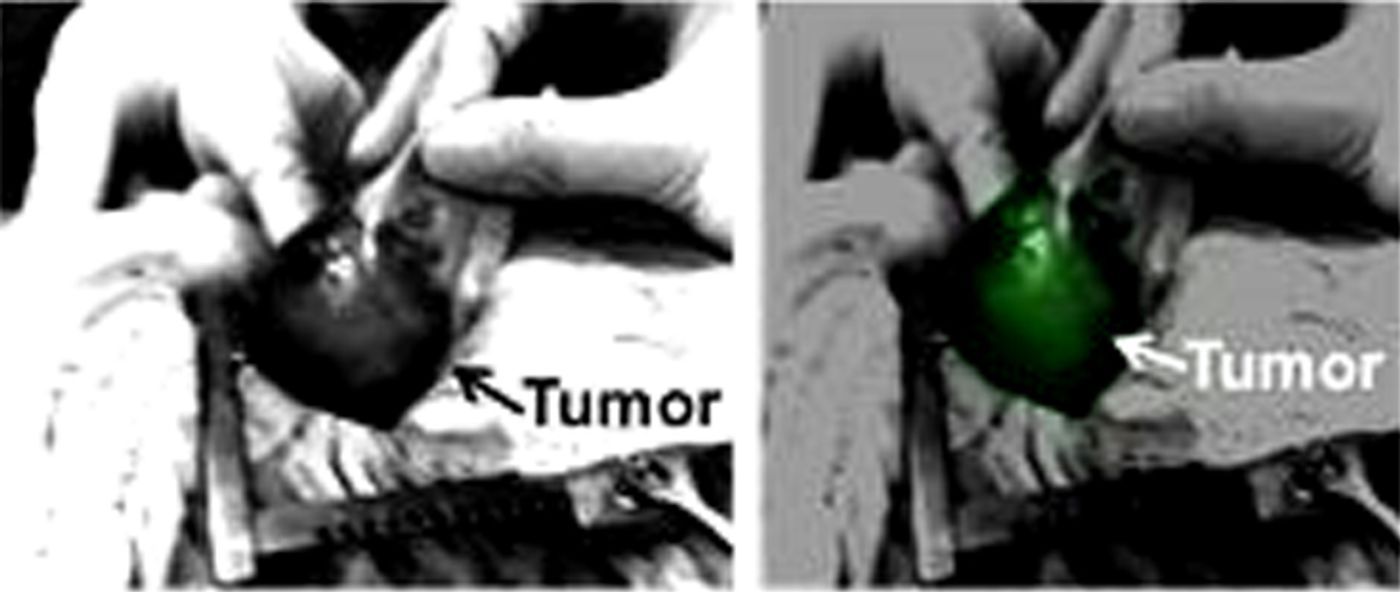
To circumvent cancer’s ability to camouflage itself among normal tissues, Penn researchers set out to make cancer as visible as possible to the surgeon. Specifically, they engineered a dye that collects mostly in the tumor tissues, making the cancer glow brightly as compared to the healthy tissues.
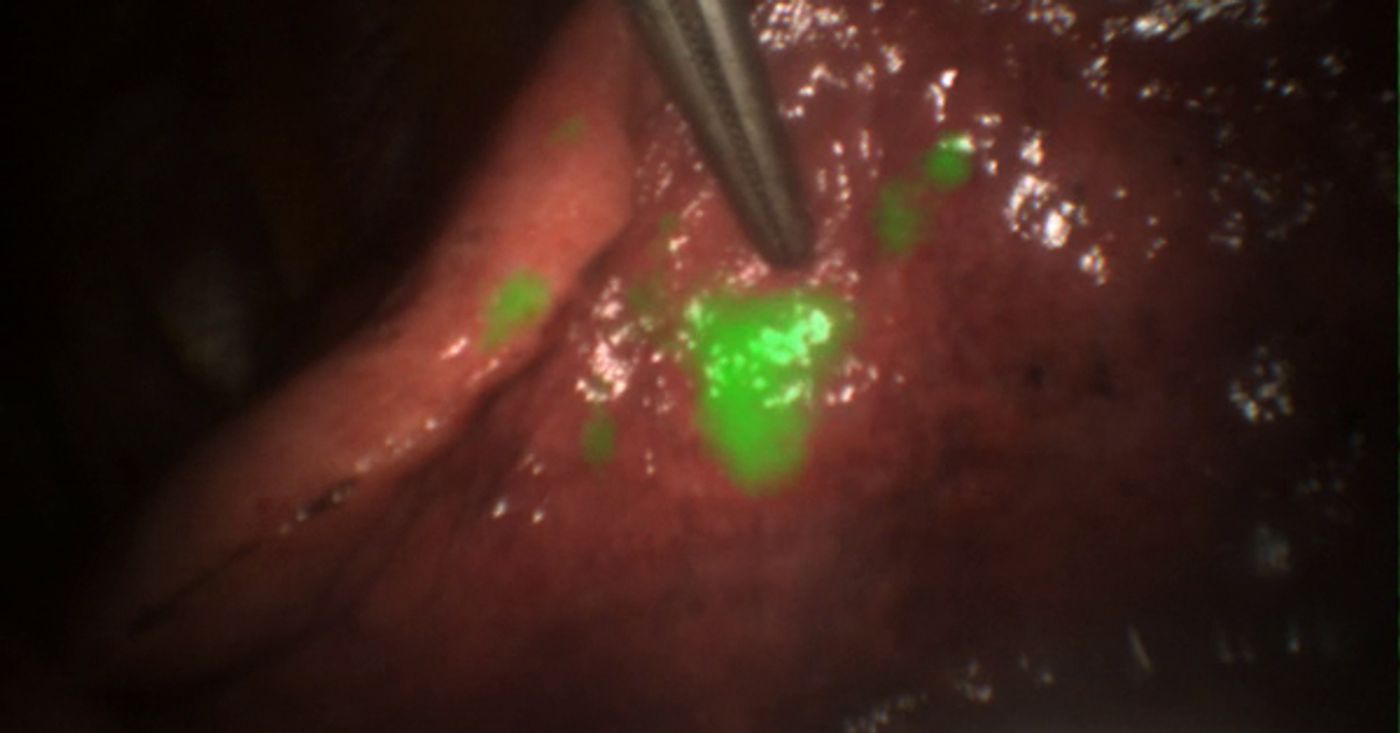
The dye agent is known as indocyanine green (ICG), and it is visualized with near infrared imaging light. "Fluorescent contrast agents take visualization to a whole new level," said John Lee, associate professor at the University of Pennsylvania’s School of Medicine. "It has the potential for real-time imaging, identification of disease, and most importantly, precise detection of the tumor's margins. With this, we know better where to cut."
The concept of making tumors glow is not new. Last month, doctors from Seattle Children’s Hospital used a chemical called BLZ-100 Tumor Paint to aid in the removal of a brain tumor in a 2-year-old. Of note, both techniques employ the use of the dye, indocyanine green.
In the current pilot study at Penn, researchers say their technique showed successful visual enhancement in 12 out of 15 tumors. Of those patients in which the fluorescence signal was strong, surgeons reported the glow was visible even under the dura.
"This technique, if approved by the FDA, may offer great promise to physicians and patients," Singhal said. "It's a strategy that could allow greater precision across many different cancer types, help with early detection, and hopefully better treatment success."
Additional sources:
Perelman School of Medicine at the University of Pennsylvania
 The dye agent is known as indocyanine green (ICG), and it is visualized with near infrared imaging light. "Fluorescent contrast agents take visualization to a whole new level," said John Lee, associate professor at the University of Pennsylvania’s School of Medicine. "It has the potential for real-time imaging, identification of disease, and most importantly, precise detection of the tumor's margins. With this, we know better where to cut."
The dye agent is known as indocyanine green (ICG), and it is visualized with near infrared imaging light. "Fluorescent contrast agents take visualization to a whole new level," said John Lee, associate professor at the University of Pennsylvania’s School of Medicine. "It has the potential for real-time imaging, identification of disease, and most importantly, precise detection of the tumor's margins. With this, we know better where to cut."