Reversing Type 1 Diabetes in Humans and Pets
Researchers at Purdue University and the Indiana University School of Medicine may have found a surprising new way to relieve diabetes. By combining pancreatic cells with a protein called collagen, scientists at Purdue University were able to reverse the symptoms of type 1 diabetes by injecting the cocktail under the skin. Pre-clinical tests showed that treatment was effective for 90 days or more. This therapy may be useful for humans as well as dogs.
This work has been reported in the American Journal of Physiology - Endocrinology and Metabolism, and a clinical study using diabetic dogs is now planned with the College of Veterinary Medicine at Purdue. It is outlined in the video.
"We plan to account for differences from mouse to human by helping dogs first. This way, the dogs can inform us on how well the treatment might work in humans," noted graduate researcher Clarissa Hernandez Stephens of Purdue's Weldon School of Biomedical Engineering. Findings.
Around one of every hundred pets and 1.25 million people in the US are thought to have type 1 diabetes, in which insulin levels have to be carefully monitored and controlled. "With giving my dog shots twice a day, I have to constantly be thinking about where I am and when I need to be home. It greatly affects my work and my personal life," said Jan Goetz, owner of a diabetic dog named Lexi. "Not having to give these shots would mean freedom."
"A type 1 diabetes diagnosis was my 18th birthday present, and since that first insulin injection, managing diabetes has been my 'other' full-time job," said patient David Taylor. "Treatment methods have improved enormously over 50 years, but they still permit no time off for the patient. Receiving an injection every few months would restore the near-normal life to me that I haven't had as an adult - and I could retire from that full-time diabetes management job."
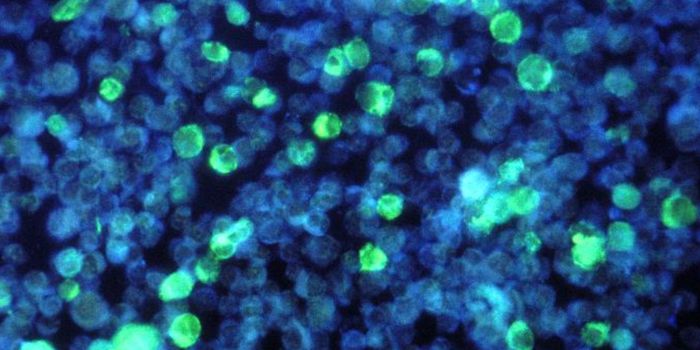
Pancreatic cells that make insulin are destroyed in type 1 diabetes, and a new set of those cells may benefit diabetics. So far, such a therapy has proven to be easier said than done.
"Traditionally, we transplant islets in the liver of the animal and never do it under the skin, in large part because the skin doesn't have the blood flow that the liver has for transporting insulin released by islets. And there are a lot of immune cells in the skin, so chances of rejection are high," explained Raghu Mirmira, professor of pediatrics and medicine and director of the Diabetes Research Center at the Indiana University School of Medicine.
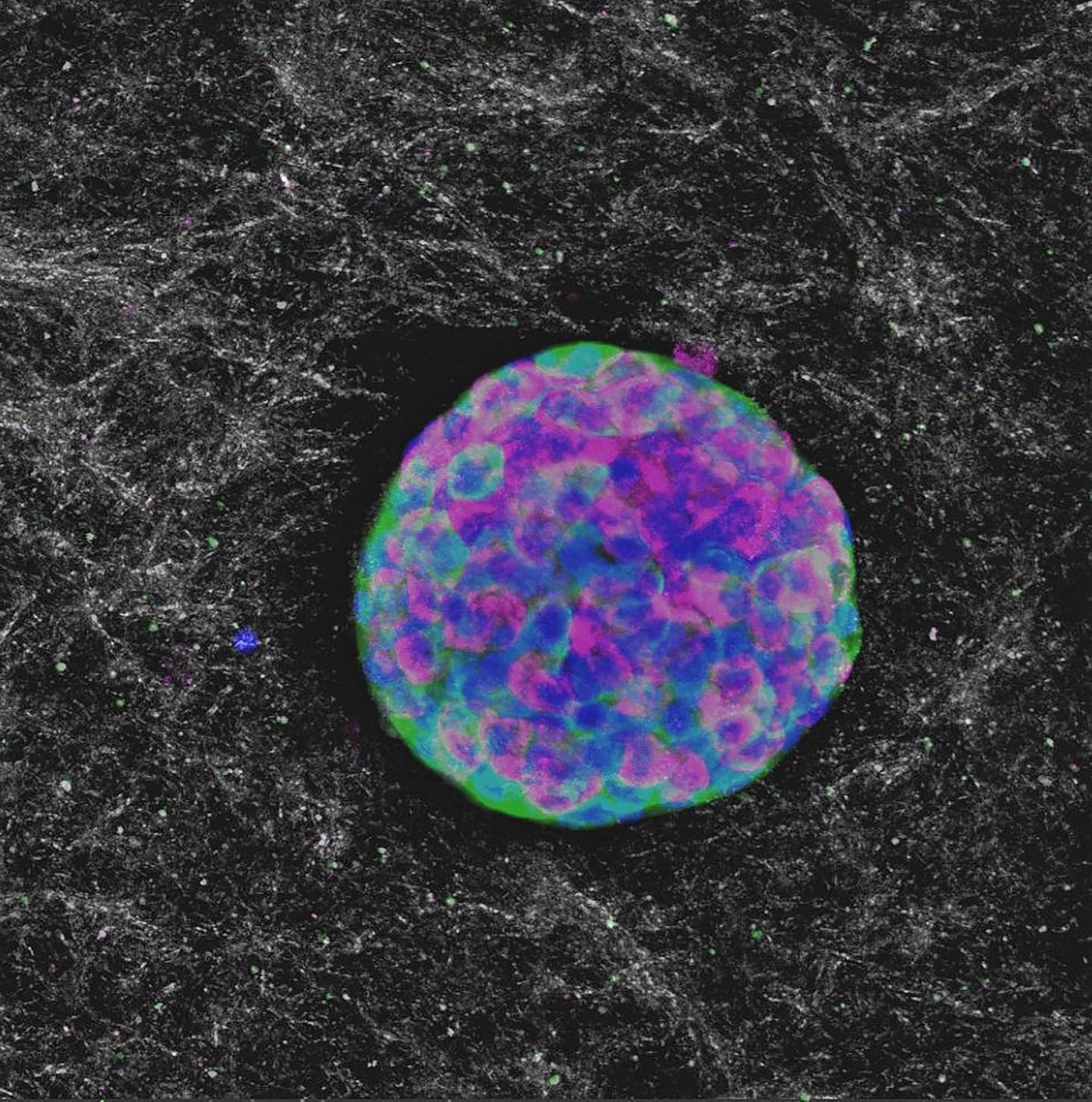
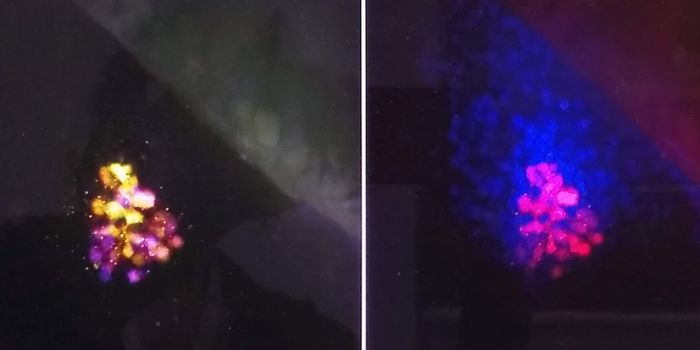
The researchers improved the procedure by packaging the islets with a solution that contained collagen, a structural protein. They injected through the skin instead of the liver to test this less invasive process. The collagen solution solidified after injection, and the body supplied the cells with blood. That allows for the exchange of insulin and glucose.
"It's minimally invasive; you don't have to go to the operating room and have this infusion into the portal vein. It's as easy as it comes, just like getting a shot," noted Sherry Voytik Harbin, Purdue professor of biomedical engineering and basic medical sciences.
More work remains, but this could be the beginning of a powerful new therapeutic option for diabetics and diabetic pets.
Sources: AAAS/Eurekalert! Via Purdue University, American Journal of Physiology - Endocrinology and Metabolism