Tumors Eradicated by Immune-stimulating Agents
With mice as a model, researchers at Stanford discovered that by injecting two molecules that stimulate the immune system, solid tumors and any trace of cancer could be eliminated. This T cell activating therapy could work for many types of cancer. Because only small amounts are needed in a targeted approach, the researchers believe this could be an affordable treatment that doesn’t cause as many side effects as other therapeutics.
“When we use these two agents together, we see the elimination of tumors all over the body,” noted Ronald Levy, MD, professor of oncology. He was senior author of a report in Science Translational Medicine summarizing the findings. “This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
One drug is already approved for human use, and the other has undergone testing for human patients in a few unrelated clinical trials. This January, a new clinical trial was launched to assess this treatment in lymphoma patients.
There has been considerable interest in developing drugs that use the immune system to fight cancer. Some approaches rely on bodywide stimulation; others remove a patient’s immune cells and genetically alter them to combat cancer before reinjecting them. While there have been other attempts as well, none have been entirely successful. Some are very expensive or laborious; others cause serious side effects.
“All of these immunotherapy advances are changing medical practice,” Levy said. “Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself. In the mice, we saw amazing, bodywide effects, including the elimination of tumors all over the animal.”
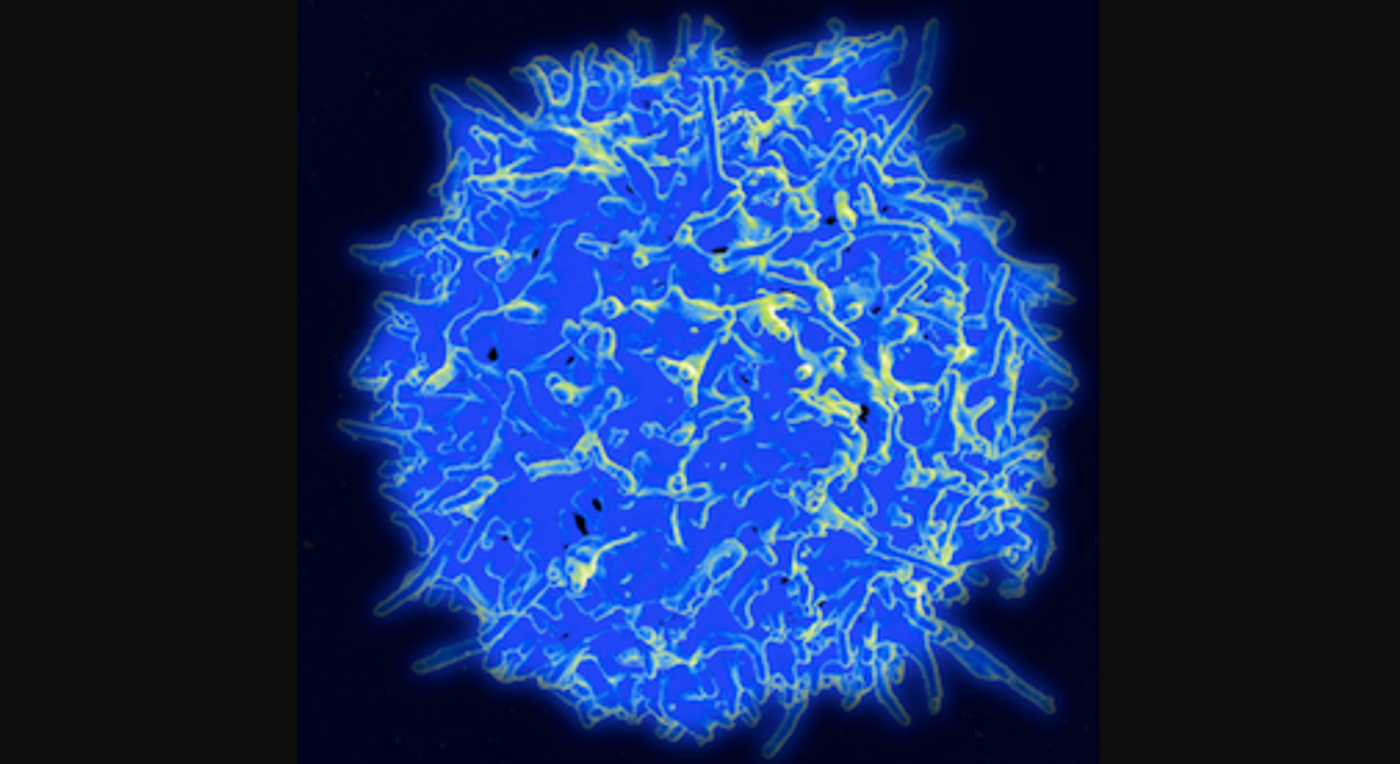
Typically, cells of the immune system that should recognize foreign invaders, T cells, will attack cancer cells at first, but as cancerous tumors grow, they are often able to suppress T cell activity.
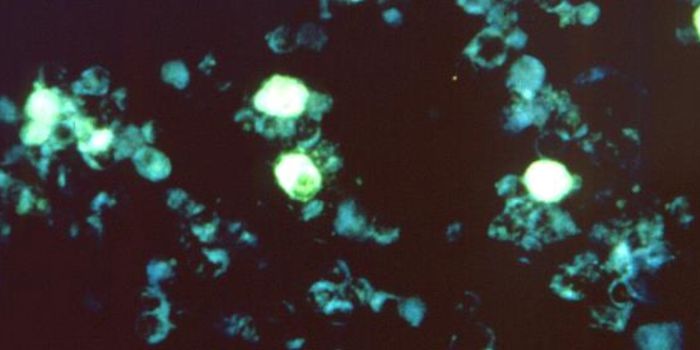
Levy’s team aimed to stimulate T cells that target cancer by exposing them to minuscule amounts of two agents at the site of tumors. One is a short snippet of DNA called an oligonucleotide; it boosts the expression of a T cell receptor. The other molecule is an antibody that binds to that receptor. Together, the antibody and receptor team up to activate the T cells. Only T cells that have gotten into the tumor are activated since the agents are applied to the tumor directly. Those T cells can recognize a specific cancer, and some leave the site of the tumor. They then migrate throughout the body and destroy other, similar tumors.
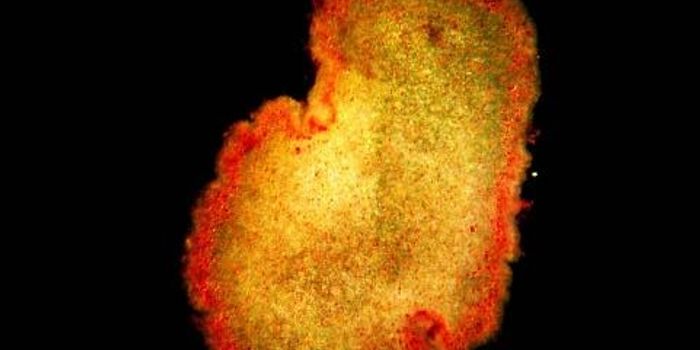
This was a remarkably effective approach that worked in transplanted lymphoma tumors, with both the original injected tumor getting destroyed as well as a second, uninjected tumor. The therapy also worked on genetically engineered mice that develop breast cancer. In the cases of cancers that grew back after the first treatment, a second treatment removed it again.
After testing mice that had been transplanted to receive lymphoma tumors and colon cancer, the treatment eliminated the lymphoma tumors, but not the colon cancer.
“This is a very targeted approach,” Levy explained. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
If the current trial, which will have around fifteen lymphoma patients, is successful, the researchers want to find out if it works with other kinds of cancer.
“I don’t think there’s a limit to the type of tumor we could potentially treat, as long as it has been infiltrated by the immune system,” Levy said.
Sources: Stanford University, Science Translational Medicine