Glowing Tumors Reveal How Immunotherapeutics Work
In a study published in the Journal of Clinical Investigation, researchers used positron emission tomography (PET) scans to examine how an immunotherapy drug reaches a tumor and the parts of a cancer that remain unaffected.
Learn more about how PET scans work:
The process of PET imaging uses a synthesized radiolabeled protein that locks on to tumor cells—this allows researchers to visually follow where the so-called checkpoint inhibitor drug binds to a tumor. "This approach offers a vital step toward directly measuring how well immunotherapy drugs are able to engage a tumor in any given person," says Sridhar Nimmagadda, Ph.D., associate professor of radiology and radiological science at the Johns Hopkins University School of Medicine and a member of the Sidney Kimmel Comprehensive Cancer Center.
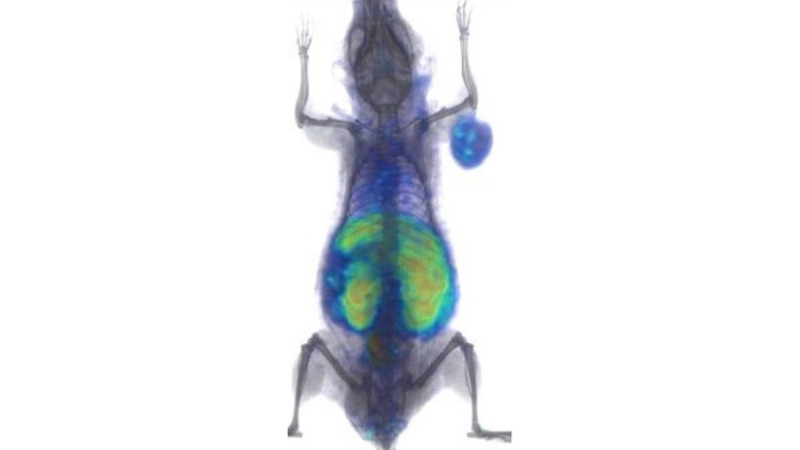
Radiolabeled protein lights up tumor implanted in the arm of a mouse under a PET scan. The researchers hope to use scans like this one to calculate in real time how much of an immunotherapy drug reaches a tumor and what parts of a cancer remain unaffected. Credit: Sridhar Nimmagadda via John Hopkins
If PET imaging precision is confirmed to be highly effective in additional tests, it could streamline cancer therapy by enhancing the therapeutic dose of a drug. The use of checkpoint inhibitors is a form of cancer therapy designed to help the immune systems recognize cancer cells and to target them. For example, the programmed death ligand 1 (PD-L1) is one such checkpoint target by three approved therapeutics called atezolizumab, avelumab and durvalumab by the U.S. Food and Drug Administration (FDA).
In the study, researchers created a radiolabeled small protein that binds to PD-L1 which facilitates marking its receptor with a radiotracer seen with PET imaging technique. "In human patients, this could give us some insight about how to optimize further treatments by increasing the dose or substituting other drugs or therapies more quickly,” says Nimmagadda.
Source: John Hopkins School of Medicine