Functional Mini-Livers Made With New Bioprinting Technique
Many people are waiting for new organs, and some die before they get one. Bioprinting might help eliminate the need for organ donors one day, and researchers are trying to get closer to that goal. Brazilian scientists have now used human blood cells to generate miniature versions of the liver (liver organoids) that are capable of doing what a normal liver typically does. They can make important proteins, store vitamins and secrete bile, for example. By reprogramming genes in adult cells to create stem cells, liver tissue can now be produced by a lab bioprinter in only 90 days. In this study, reported in Biofabrication, the tissue maintained its functions for longer than any previous effort.
"More stages have yet to be achieved until we obtain a complete organ, but we're on the right track to highly promising results. In the very near future, instead of waiting for an organ transplant, it may be possible to take cells from the patient and reprogram them to make a new liver in the laboratory. Another important advantage is zero probability of rejection, given that the cells come from the patient," noted the senior study author Mayana Zatz, director of the Human Genome and Stem Cell Research Center.
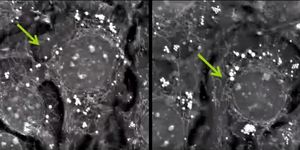
In this work, cells were put into a bioink so the printer could generate the tissue. "Instead of printing individualized cells, we developed a method of grouping them before printing. These 'clumps' of cells, or spheroids, are what constitute the tissue and maintain its functionality much longer," explained the first study author Ernesto Goulart, a postdoctoral fellow at the University of São Paulo’s Institute of Biosciences.
Cells slowly lose contact in typical bioprinting techniques, thereby causing the loss of function. Live tissue has previously been printed by putting cells into a hydrogel and dispersing them.
"It's a somewhat traumatic process for the cells, which need time to get used to the environment and acquire functionality," Goulart said. "At this stage, they aren't tissue yet because they're dispersed, but as shown by our study, they already have the capacity to clear the blood of toxins and to produce and secrete albumin [a liver protein], for example."
Pluripotent stem cells can become any type of specialized cell and in this work they generated liver tissue cells: hepatocytes, mesenchymal, and vascular cells, which began to form spheroids. "We started the differentiation process with the cells already grouped together. They were cultured in agitation, and groups formed spontaneously," Goulart explained.
After collecting a patient’s blood, it would take about 90 days to make functional tissue, the researchers said. The cells have to be genetically reprogrammed to gain pluripotency, then they must be differentiated into liver cell types. Spheroids form and are then combined with a bioink to print out structures. These structures are then grown in culture for eighteen days.
"The printing process entails the deposition of spheroids along three axes, which is necessary for the material to gain volume and give the tissue proper support," Goulart said. "The gel-like bioink is crosslinked to make the structures more rigid so that they can be manipulated and even sutured."
This study created mini-livers by collecting blood cells from three volunteers. "Our spheroids worked much better than those obtained from single-cell dispersion. As expected, during maturation, the markers of hepatic function were not reduced," Goulart said.
While only miniature livers were made, the researchers suggested that this technique could be useful in the production of complete organs that can be transplanted into patients. "We did it on a small scale, but with investment and interest, it can easily be scaled up," Goulart said.
Sources: AAAS/Eurekalert! via São Paulo Research Foundation (FAPESP), Biofabrication