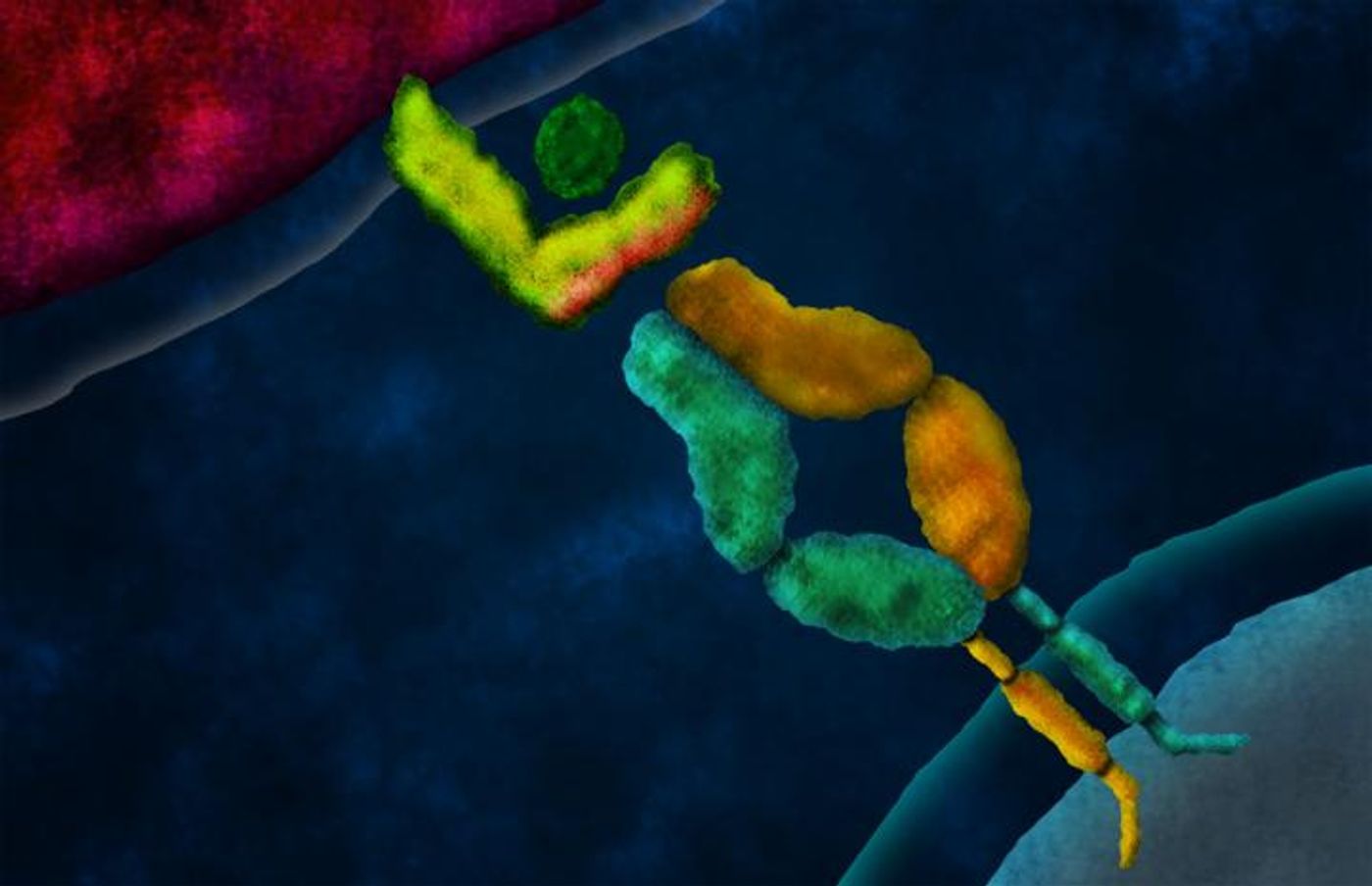
Scientists are hard at work improving immune cells called T cells, which are naturally designed to recognize and target foreign invaders. They are vulnerable to error, though, and tinkering with their cell components can often reduce the amount of mistakes they make. A new technique developed from scientists at the California Institute of Technology now produces the best-ever engineered T cells that can be used to treat cancer.
T cells are unique. Each immune cell as a T cell receptor (TCR) that recognizes specific antigens, so two T cells with different TCRs recognize different antigens and are used to fight different diseases. The specificity of an individual T cell is written by the pairing of two protein chains: alpha and beta. The two chains both have domains that are “constant” and “variable,” meaning domains that are reserved throughout all T cells and domains that are unique to one specific T cell, respectively.
Cells specifically designed to present antigens to T cells gather parts of a foreign cell to present to T cells for analysis. If a T cell deems the antigen worthy of attack, whether it’s pathogenic or cancerous, an immune response ensues. Therefore, without the effectiveness of the TCR, T cells cannot accurately recognize antigens that need to be attacked. Demonstrated in the new technique from CalTech, scientists have developed immunotherapies to boost the immune response as a way to treat cancer.
The new technique, called domain swapping, was developed in the laboratory of David Baltimore, president emeritus and the Robert Andrews Millikan Professor of Biology. But before domain swapping, there was TCR gene therapy.
TCR gene therapy was implemented to take control over TCR recognition of antigens by manually inserting genes encoding a specially-designed target to a particular tumor cell type. This experimental therapy resulted in T cells that expressed two alpha chains and two beta chains, meaning four possible pairings, rather than natural T cells that express just one of each chain.
While this technique did provide scientists the capability to create an army of specialized T cells to target a specific type of cancer, certain risks also accompanied the new technology. Autoimmunity occurred as a serious side effect, after genetically-inserted TCR chains intertwined with the innate receptors already present in the T cell. This reaction caused T cells to attack healthy cells that were neither cancerous nor pathogenic.
"As T cells are produced, the immune system 'auditions' them, eliminating those that react to healthy cells and selecting those with potential to recognize diseased cells," said lead author Michael Bethune, PhD. "However, in T cells engineered to express a second TCR, the introduced chains can mispair with the resident chains, resulting in TCRs with unintended and unpredictable specificity. These mispaired TCRs are not auditioned by the immune system, and some will target healthy cells causing autoimmunity."
Bethune and his team fixed the failures of TCR gene therapy to create the domain swapping technique, which is void of the dangerous autoimmune reactions. Whereas 90 percent of mice given TCR-engineered T cells via TCR gene therapy exhibited autoimmune reactions, domain swapping proved to be a much safer, autoimmune-free treatment.
Domain swapping bypassed autoimmunity because of hybrid genes Bethune and his team manufactured in the lab. These genes encode TCR chains with alpha and beta constant domains already swapped in a “compensatory fashion.” The new domain swapping technique, Bethune said, “ensures that only the correctly paired domain-swapped TCRs function at the surface of the cell.”
With his findings, Bethune has created essentially the most error-free technique for genetically engineering top-notch T cells to target cancer. In the future, this technique could be personalized to individual cases of cancer, creating T cells specifically designed to fit a patient’s needs.
The present study was published in the journal
eLife.
Source:
California Institute of Technology