The Problems & Potential of Precision Medicine
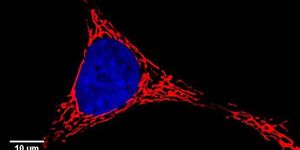
In cancer diagnostics and therapeutics, genetic testing is used to guide doctors to the best treatments and most effective drugs for patients. This so-called precision medicine aims to identify genetic mutations that are driving cancer development and the targeted drugs that can treat them. A study by led by the Translational Genomics Research Institute (TGen) and the Keck School of Medicine of the University of Southern California (USC) has found that such medicine is actually not that precise when used for more diverse populations.
In an ideal situation, a tumor from a patient as well as a sample of normal tissue is used to identify mutations that are tumor-specific. But a healthy sample is not always available, and genetic material from only the tumor is obtained. Population databases then have to be used to fill in for a normal sample, rather than healthy patient DNA. Because so much more population data is available for those of European ancestry, this approach is far less precise when applied to those of Latin American, African and Asian descent, according to work in the journal BMC Medical Genomics.
The research team wanted to create a computational tool to find variations in the genome that may cause cancer, so there will be an alternative to looking at population data only. Their new tool, LumosVar, is a big improvement, but cannot yet identify the ideal drugs for each individual with cancer.
"The field of precision medicine isn't taking into account population differences. The approaches being used are imprecise when you look at very specific populations," explained a lead author of the work, Dr. John Carpten, Director of the Institute of Translational Genomics at the Keck School of Medicine of USC.
"It is very difficult to identify a somatic, or potentially cancer-causing, variant when you don't have a germline, or normal, sample," said Dr. Rebecca Halperin, a TGen Assistant Research Professor and the other lead author. "It's even worse, depending on your ancestry. You get more false positives -- those genetic variants that don't cause cancer -- from populations with non-European ancestry."
Not only has most genetic data come from those of European descent, European ancestry is the least diverse. The most diverse genomes come from those in Bangladesh, while the least diverse come from Scandinavia, not necessarily a surprising finding when one considers geography. Sequencing more individuals from more areas will be necessary; there is, even more, work to be done.
"Simply sequencing more individuals from various populations is not enough. We really need access to the germlines. But when those aren't available, we need better tools and this is where we have put our focus," stressed Dr. David W. Craig, Vice Chair of the Keck School of Medicine of USC's Department of Translational Genomics and the study's senior author.
"There is a growing body of knowledge on the shortfalls of Precision Medicine," noted Dr. Rick Kittles, Professor and Founding Director of the Division of Health Equities, Department of Population Sciences, at City of Hope, and one of the world's foremost scientists in the area of population genetics and cancer.
This problem is a serious one; patients risk misdiagnosis. "That means you might be getting the wrong therapy simply because of our lack of understanding of the genetic architecture based on one's ancestry," Dr. Craig said. "These findings argue that we're really not doing a very good job of doing Precision Medicine for many populations."
"Tumor-only sequencing in patients from populations that have undergone rapid expansion significantly decreases the precision of Precision Medicine,” added Dr. Carpten. Importantly, the greater impact will be on individuals from underrepresented communities."
The LumosVar tool has been made openly accessible so that researchers and doctors can use it if they are looking for cancer-causing mutations. It is one step towards improving our ability to identify mutations that cause cancer rapidly so they can be targeted.
Learn more about precision medicine from the video by UCSF.
Sources: AAAS/Eurekalert! Via TGen, BMC Medical Genomics