Novel Immunotherapy Reduces Bone Metastasis
Triple negative breast cancer (TNBC) is usually detected at later stages. Unfortunately, by this time the cancer has moved or metastasized to other tissues throughout the body. One of the most common sites of TNBC metastasis is within the bone marrow. Bone metastasis cannot be cured and is linked to high mortality rates. Although treatments for breast cancer have improved with advances in immunotherapy, and other targeted treatments, limited efficacy is still an obstacle in late-stage tumors. As a result, scientists and physicians are working to understand the inter-play between different cell types in the metastatic environment, commonly referred to as the “metastatic microenvironment”. One major obstacle includes immunosuppressive cells within the tumor and metastatic microenvironment that limit anti-tumor immune cells, known as T cells. The complex interaction between these immunosuppressive cells and T cells prevents the immune system from recognizing and killing the tumor. Consequently, the tumor progresses and metastasizes to the bone and continues to spread unless treated. Scientists and physicians and working to reduce and eventually prevent bone metastasis through different therapeutic regimens offered in the clinic.
A recent paper from Cancer Discovery, by Dr. Neta Erez, demonstrated that immunosuppressive cell targeted therapy overcomes immunotherapy resistance in bone metastatic TNBC. Dr. Erez is a Professor and Vice Dean at the Tel Aviv University in the School of Medicine. Her work focuses on the complex tumor microenvironment and how different cells interact to promote tumor growth. The goal of her lab is to understand these processes and overcome them using therapeutic approaches.
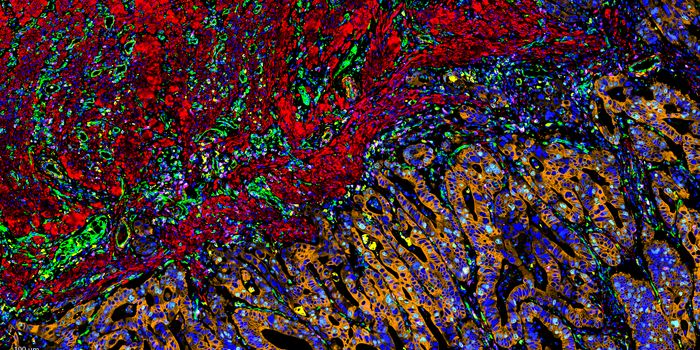
Researchers first established that T cells highly infiltrate the bone metastatic environment. Different T cell subtypes associated with immune suppression were present in the bone marrow due to other immunosuppressive cell types, particularly granulocytic myeloid-derived suppressor cells (G-MDSCs). These G-MDSCs restricted T cells from proliferating and targeting tumor cells. The team used next generation sequencing to analyze the G-MDSCs and found they have upregulated markers indicative of an immunosuppressive function. One upregulated protein found to generate suppressive G-MDSCs was IL1β. IL1β is a protein which was linked to the progression of TNBC metastasis. Erez and others next wanted to understand how G-MDSCs physically blocked T-cells from killing the tumor.
Researchers found that markers known to bind to G-MDSCs, T cell immunoreceptor with immunoglobulin and ITIM domain (TIGIT), were highly expressed on T cells. The interaction between G-MDSCs and T cells bound with TIGIT was highly upregulated in the bone metastatic environment. Therefore, Erez and her team treated mice with TNBC bone metastasis with an antibody targeting the development of G-MDSCs (anti-IL1β) with an immune checkpoint inhibitor (anti-TIGIT). The combination of targeted therapy and immunotherapy resulted in significant reduction of bone metastasis and improved survival. Additionally, the team discovered similar patterns in human samples across different cancer models including colorectal, lung, and prostate cancer. This suggests that the combination treatment may improve overall survival in late stage TNBC. Further work must go into testing this regimen in clinical trials, but the paper clearly demonstrates the efficacy of this drug combination and the mechanism that drives bone metastasis.