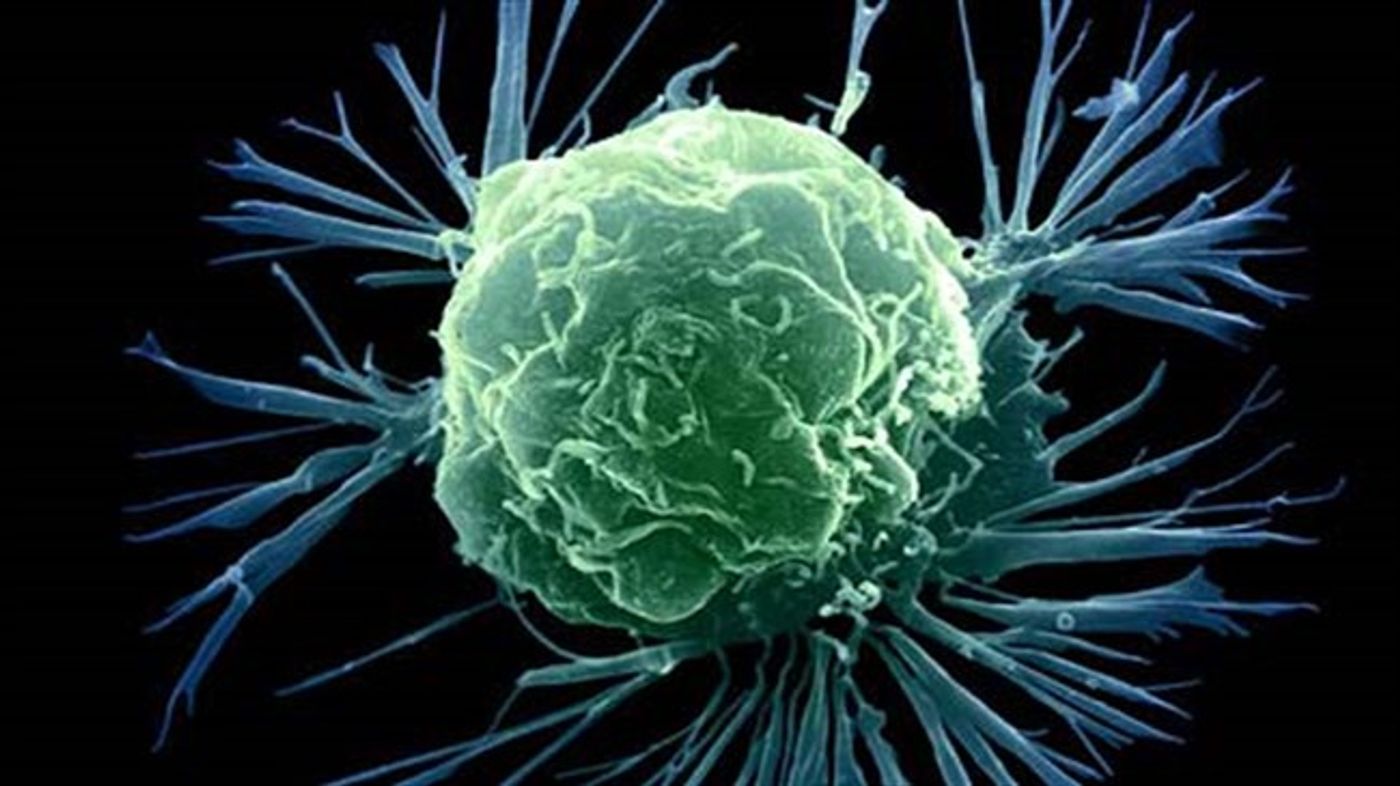
TSRI Researchers Believe Cell Population May Provide a New Cancer Drug Target
LA JOLLA, CA – November 11, 2016 – A new study led by scientists at The Scripps Research Institute (TSRI) suggests there may be a way to limit tumor growth by targeting immune system cells called macrophages.
The research reveals that macrophages can “drill” through tumors to create new vessel-like structures for delivering oxygen and nutrients as tumors grow.
“This may represent a whole new therapeutic target for treating tumors,” said TSRI Professor Martin Friedlander, senior author of the new study, which was published November 11 in the journal Scientific Reports.
A Different Kind of Vessel
Blood vessels are normally built by endothelial cells. In cancer, tumor cells can induce endothelial cells to build new vessels to bring in blood rich with oxygen and nutrients, a process called angiogenesis.
Recent research has revealed that not all vessels are lined by endothelial cells. In cancer, vessel-like structures can be created by a non-endothelial cell type. This phenomenon, called “vascular mimicry,” has been observed in several types of solid tumors, including glioblastoma, breast cancer and melanoma, and has been attributed to a sub-population of cells within the tumor called cancer stem cells.
Yet the scientists in this study found that macrophages can form vascular mimicry channels in tumors, as well as in other low-oxygen environments. Although macrophages are key cells of the immune system that recognize and attack foreign invaders and cancer cells, macrophages can be re-programmed within the tumor environment to promote tumor growth.
The scientists in the new study presented a new and unrecognized structural role for macrophages in the formation of a vascular mimicry network connected to the systemic circulation.
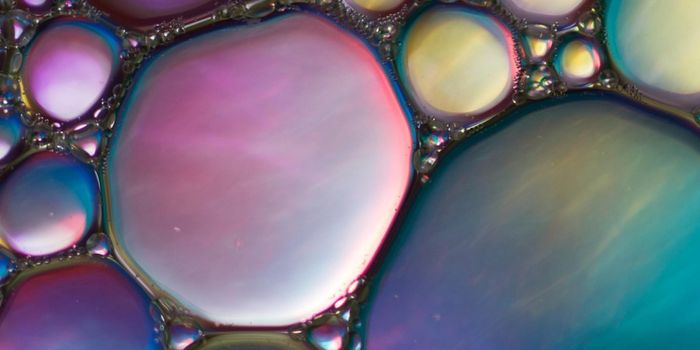
“These conduits have an architecture distinct from that of traditional blood vessels,” said Faith H. Barnett, a cancer researcher and neurosurgeon at Scripps Clinic who served as co-first author of the study with Mauricio Rosenfeld.
Using an intravenously injected dye to delineate the established vasculature as well as the newly formed vascular mimicry conduits, the researchers found that macrophages quickly migrate to oxygen-deprived environments and form these vessel-like channels. Experiments spearheaded by Barnett and Rosenfeld showed that these tubular structures are lined with cells that express macrophage cell surface markers.
“Macrophages are capable of forming a three-dimensional network,” said Rosenfeld.
These vessel-like channels appeared too small to carry red blood cells, but the researchers believe that the low oxygen concentrations within tumors drive macrophages to form this network of channels to transport dissolved oxygen and glucose.
A Possible Cancer Target
The findings could explain why current drugs to slow angiogenesis do not slow tumor growth in some patients. Friedlander said future cancer therapies could starve tumors by combining current vessel-targeting drugs with drugs to influence macrophage activity.
“There may be an opportunity to intervene therapeutically,” Friedlander said.
In addition to providing a new approach to cancer, Friedlander added that future studies could focus on better understanding how macrophages influence retinal angiogenesis and blood flow in the eye—a key concern for people with diseases like age-related wet macular degeneration, where leaky vessels can cause vision loss.
The researchers added that this study would not have been possible without TSRI’s core facilities scientists, who aided with electron microscopy, confocal imaging, in vivo mouse efforts and quantitative analysis.
In addition to Friedlander, Barnett and Rosenfeld, authors of the study, “Macrophages form functional vascular mimicry channels in vivo,” were Malcolm Wood, William Kiosses, Yoshihiko Usui, Valentina Marchetti and Edith Aguilar, all of TSRI at the time of the study.
The study was supported by the National Institutes of Health (grant R01EY011254).
This article was originally published on
Scripps.edu.