Relieving "Exhausted" Immune Cells To Kill Cancer
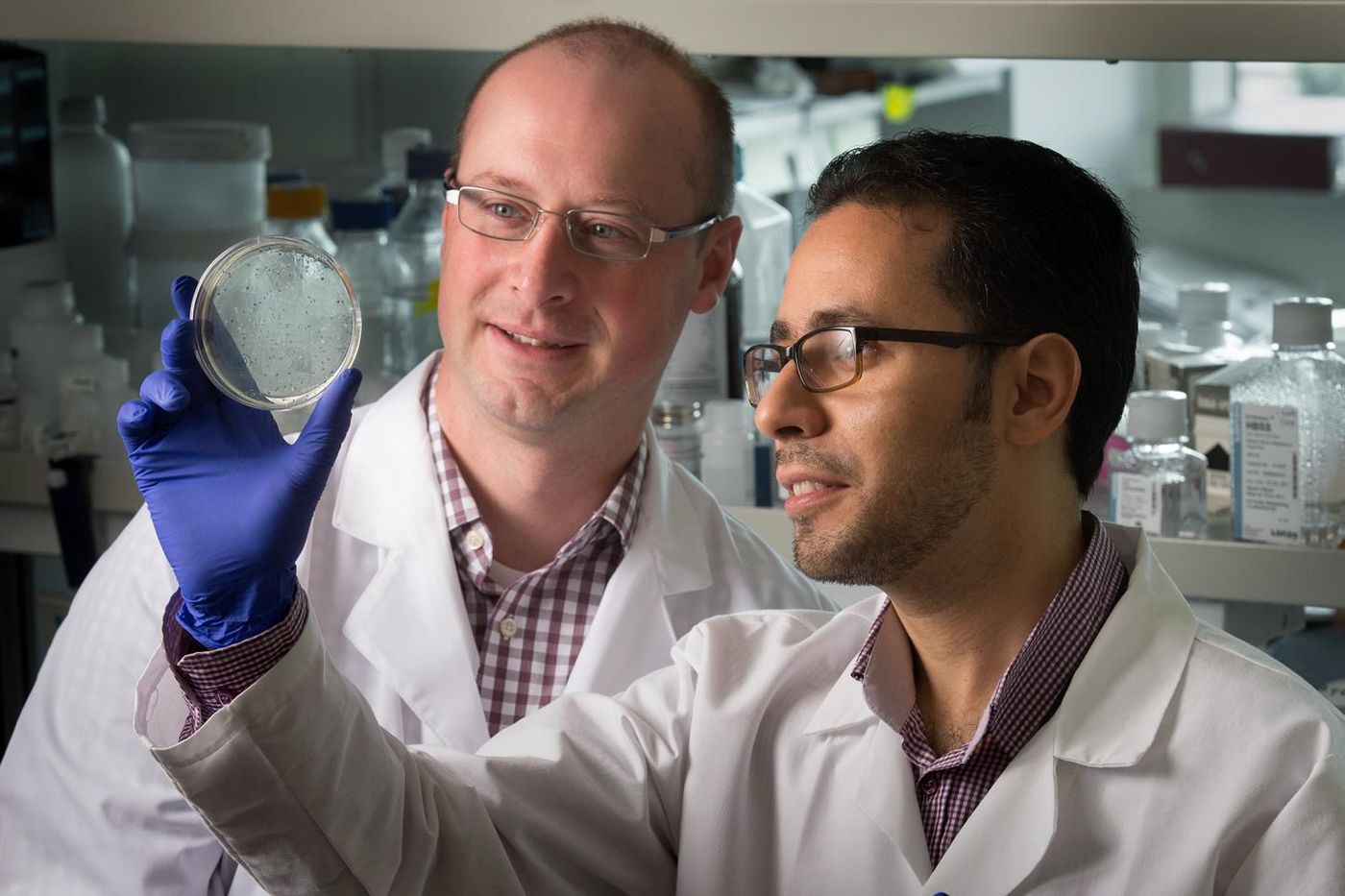
How do T cells become so “exhausted” that they can no longer effectively fight cancer, viruses, bacteria, and other invaders as they are created to do? Scientists from St. Jude Children’s Research Hospital have an answer as well as a way to overcome this exhaustion.
T cells are key players of the immune system that protect the body from an array of attacks, but when they can’t recognize foreign cells, they can’t direct the immune system to attack. With St. Jude scientists already in the process of designing techniques to rejuvenate T cells, they over the possibility of improving existing immunotherapies to reduce tumor growth, an anti-cancer strategy that relies on boosting the power of the immune system to defend itself.
When immunotherapy doesn’t reach its full potential due to T cell exhaustion, cancer often fails to respond to the treatment, or a patient quickly experiences a relapse of the disease. Researchers believe this failure is due to dysfunction of a process called the “immune checkpoint blockade.”
"The clinical significance of T cell exhaustion is huge, because when a person comes into the clinic with a tumor, it is likely they have had it for many months," explained lead researcher Ben Youngblood, PhD.. "And their T cells, which would be responding to that tumor, have been exposed to the tumor antigen for a long time. This may likely be why immunotherapy fails in many patients, because their T cells are already exhausted or stably repressed."
Youngblood’s proposed solution is based off of preclinical studies of viral infections and growing tumors, indicating a chemotherapy drug called decitabine as capable of bringing exhausted T cells back to life. Plus, the drug is claimed to have the potential to be useful against multiple types of afflictions: HIV in addition to cancer and other pathogens.
"We know the T cells in patients with HIV become exhausted," Youngblood said. "Although there are very effective drugs that reduce the viral load to undetectable levels, that therapy is costly and is not a cure. I'm optimistic that the immune system holds the ultimate promise of a cure for HIV infection, and basic findings such as ours represent one step toward that cure."
But what causes the immune checkpoint to fail leading to T cell exhaustion in the first place? Researchers found that it is an “epigenetic program” that prevented T cells from recognizing tumor cells as abnormal and requiring destruction. The epigenetic program persisted by being passed on through T cell generations. The chemotherapy drug decitabine blocks the epigenetic program preventing T cells from protecting the body from cancer.
"Now that we have shown this is an intrinsic property of T cells, it means you can pull out the T cells, treat them, and reintroduce them to attack the cancer," Youngblood explained. "With such approaches, you limit toxicity to the patient."
The present study was published in the journal Cell.