Common Fungus Might Exacerbate Bowel Disease in Some People
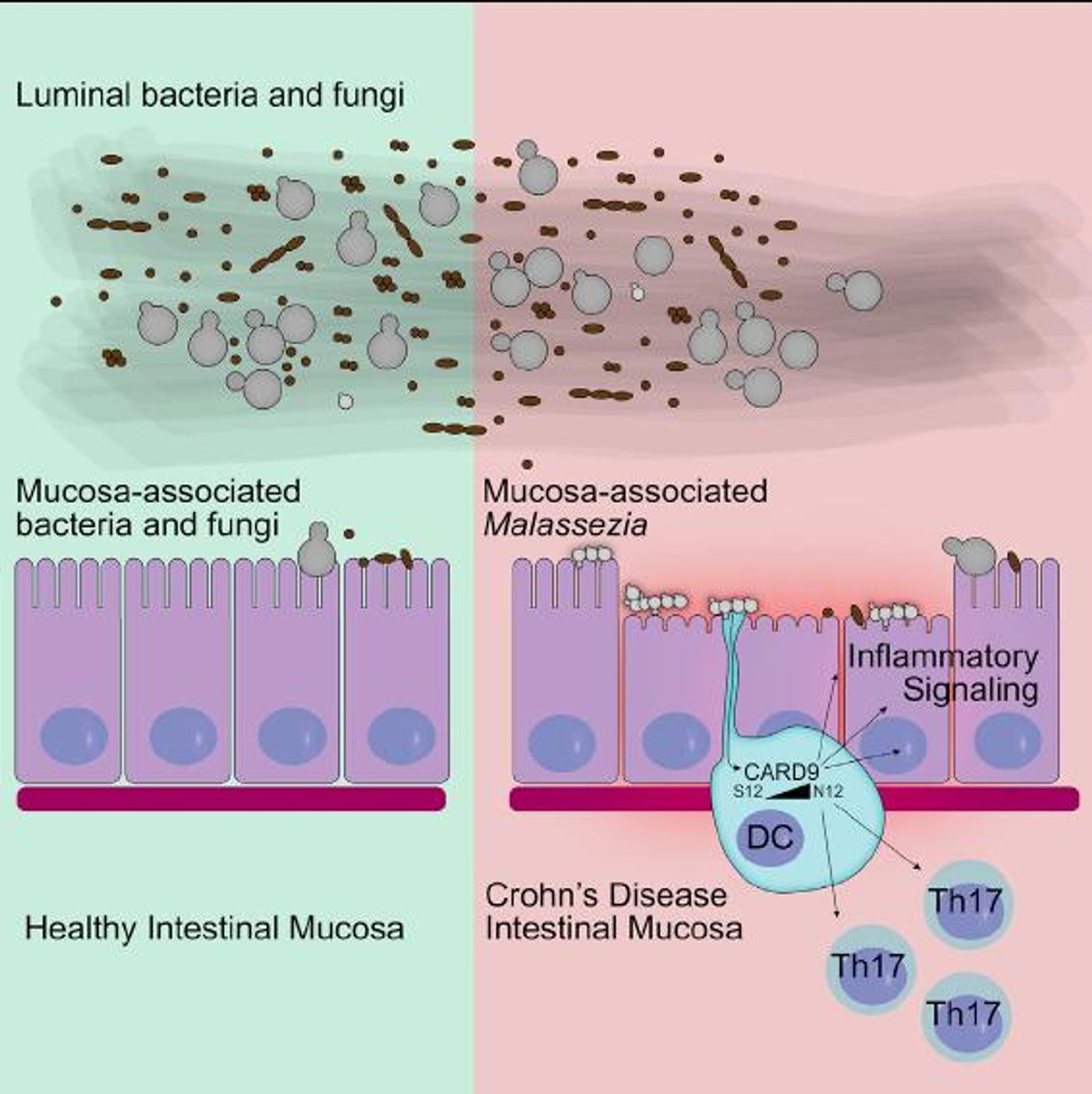
We carry around lots of microbes in and on our bodies. Our hair or oily skin might harbor a common type of fungus, Malassezia yeasts, which have been linked to skin problems like dandruff. The yeasts can end up in the gastrointestinal tract, and research indicates that it may exacerbate conditions like inflammatory bowel disease (IBD) in certain patients. The findings have been reported in Cell Host & Microbe.
“We were surprised to find that Malassezia restrica was more common on intestinal tissue surfaces in Crohn's disease patients than in healthy people,” noted study co-author David Underhill, the Janis and William Wetsman Family Chair in Inflammatory Bowel Disease at Cedars-Sinai in Los Angeles.
Our genomes are full of tiny variations in gene sequences that can lead to biological and physical changes. Some of those variants have been linked to certain conditions, and in this work, the researchers found that genetic variants seem to be encouraging the growth of Malassezia yeasts in the gut. “Further, the presence of Malassezia was linked to a common variation in a gene known to be important for immunity to fungi - a genetic signature more common in patients with Crohn's disease than the healthy population,” explained Underhill.
IBD is a condition in which the digestive tract is chronically inflamed, and refers to both Crohn’s disease and ulcerative colitis. These disorders are related to abnormal microbes in the gut, environmental changes, gene variants, and impaired regulation of the immune response. Instead of concentrating on the microbes living in the gut like many other research teams, Underhill’s group looked at how fungus might have a role in IBD.
Changes in fungi in the intestine and how the host responds to it might have a negative impact on disease in a subset of Crohn’s patients, noted study co-author, researcher Jose Limon of Cedars-Sinai.
Using a mouse model, the scientists determined that fungi in the gut microbiome can help control inflammation that arises there. In mice, the Malassezia restricta fungus made an (already present) intestinal inflammatory disease called colitis worse.
The researchers assessed fungi of the intestinal mucosa in healthy people and Crohn’s patients; they saw that several of these fungi that were present at significantly higher levels in Crohn's patients. Malassezia restricta was particularly elevated in Crohn's patients that carry a gene variant called the IBD CARD9 risk allele. That variant makes human immune cells better at getting rid of inflammatory cytokines that arise in the presence of Malassezia restricta.
“The data so far do not suggest that the presence of Malassezia in the gut is an inherently bad thing. We found it in some healthy people, and in mice it does not seem to cause disease in the gut by itself,” cautioned Underhill. “However, if there is some intestinal inflammation, Malassezia seems to make it worse.”
The researchers are now interested in Crohn’s patients would benefit from getting the yeast out of their intestinal microbiome.
Learn more from Stanford Unversity about eating well while one is dealing with Crohn's disease.
Sources: AAAS/Eurekalert! via Cell Press, Cell Host & Microbe