Understanding why the Malaria Vaccine is Ineffective in Some
Vaccines are meant to preemptively protect the body from infection, and while it is possible to produce such protective immunity against the early liver stage of malaria infection, that has been a difficult goal to reach in places that are plagued by high rates of malaria infection. Publishing their work in Cell Reports, investigators at the University of Washington (UW) School of Medicine may have found an explanation. Malaria is a virus with a complex life cycle, and the investigators found that the latter blood stage of malaria infection can inhibit the formation of protective immune cells, and their antibodies, that would otherwise prevent the early liver stage infection.
"The blood stage of malaria infection has a very profound impact on the liver stage immune response, and that impact had never been dissected and visualized at this level," said one author of the work, Marion Pepper, a researcher at UW Medicine and Assistant Professor of Immunology at the UW School of Medicine. "These studies really suggest that you need a vaccine that is protective against both stages of infection to effectively prevent malaria."
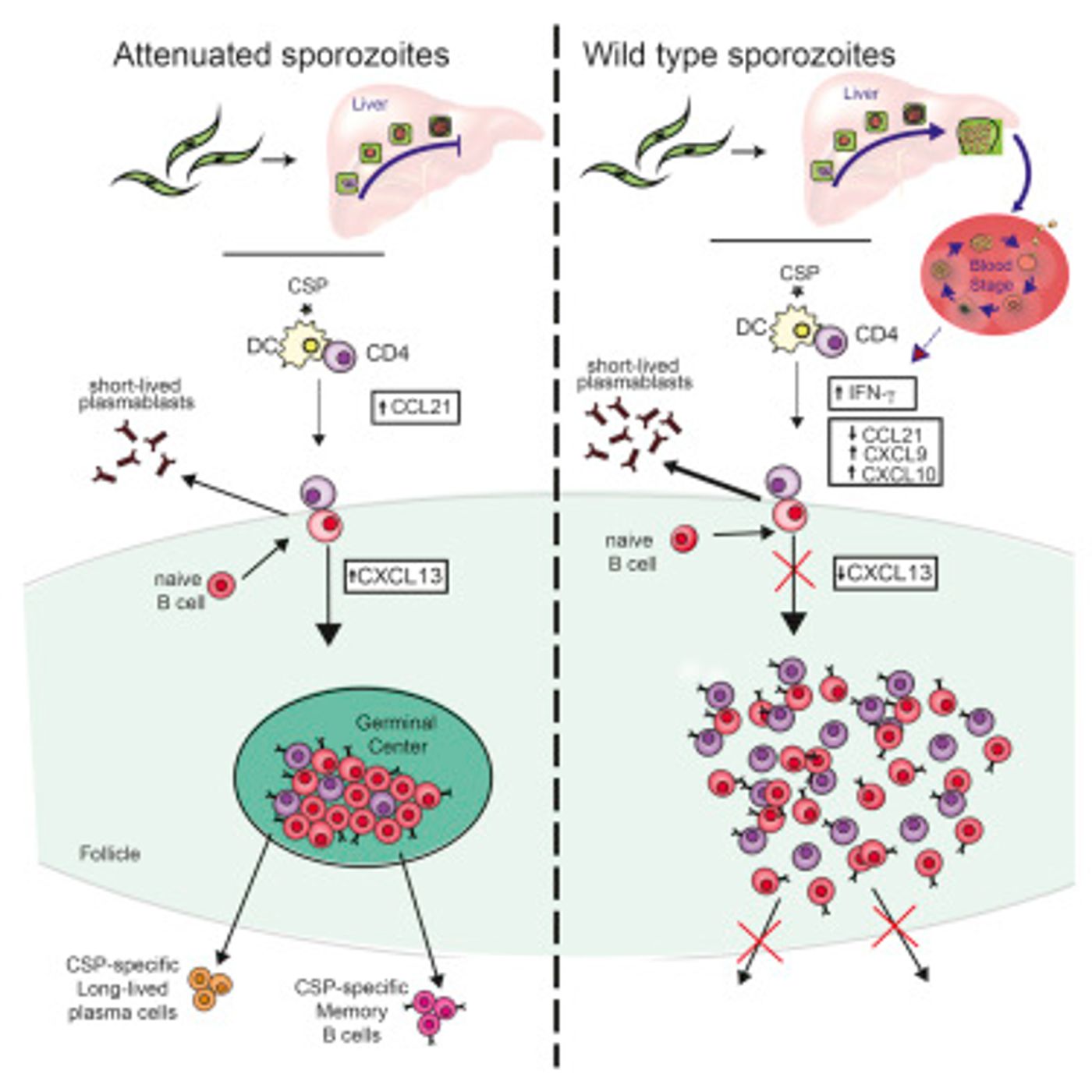
To track how the blood stage of malaria infection overpowers the liver stage immune response, Pepper’s research team studied how malaria infection at the blood stage can overpower the immune response to the liver stage with a mouse model. Two groups of mice were infected with different forms of the malaria parasite, one of which was created by study collaborators in the lab of Stefan Kappe, UW Affiliate Professor of Global Health and investigator. This form arrested when it reaches the liver infection stage; the other form continues to develop into the blood infection stage. The researchers determined that six days following infection, mice with the blood stage infection had significantly lower antibodies levels compared to mice infected with the liver-stage parasite.
The team wanted to know what was underlying that difference, so they observed Plasmodium liver stage-specific B cells differentiating - becoming a more mature or specialized cell type. B cells are able to differentiate into early effector cells, which secrete antibodies or long-lived memory cells, which can both confer protection against malaria. It was found that 14 days following infection, B cells in mice infected with blood stage malaria parasites did not follow through on the changes required for making rapidly responsive memory cells. But in mice that received the engineered, liver-stage parasite type, B cells could still differentiate, making the necessary memory cells and the antibodies that mount an effective immune response. The graphical abstract from the work is shown below.
"This work really highlights the importance of looking at antigen-specific B cells," said Pepper. "These data also suggest that if you're getting a vaccine while you have an ongoing blood stage infection, there is a chance that the vaccine will not generate good memory cells because the blood stage disrupts all the processes that are involved in making that immunological memory."
The researchers are hopeful that this problem is solvable with the right drugs since they demonstrated that show that if the second stage of the infection is treated with a drug, B cells are then able to make responsive, effective memory cells. While that could still be some time off, this work may help answer questions about malaria vaccine efficacy in areas with high infection rates.
"Malaria has evolved with us throughout human existence and therefore has some potent immune evasion strategies. We really tried to tease apart some of the factors that could be driving the loss of protective immunity during natural infection and with current vaccine strategies in areas of high malaria transmission," explained Pepper. "Our next step is to compare malaria-specific B cells after vaccination or natural infection in humans so we can translate these findings and start to determine how to solve this problem."
If you would like to know about the life cycle of the malaria parasite in a human host, check out the above video.
Sources: AAAS/Eurekalert! via Cell Press News, Cell Reports