How baroreceptors do blood pressure sensing
Winter’s up ahead, and low temperatures cause blood vessels to constrict and increase blood pressure (BP). The question is how these mechanical changes in blood vessels are translated to the brain? The BP information needs to be processed instantaneously to maintain homeostasis. It has been long known that baroreceptors, stretch-sensitive neurons in the nodose and petrosal ganglia initiate the BP regulation. However, there is an ambiguity about the specific ion channels that contribute to baroreceptor function. Do ion channels respond directly or indirectly to the mechanical changes was not clear.
Recently, ubiquitous membrane ion channels that sense mechanical stimuli in mammalians, namely PIEZO1 and PIEZO2 have been identified. The functional outreach of these channels is substantial. Neural stem cell differentiation, vasculature development during embryogenesis, sense of touch, and heart failure are just a few of the examples, where they play a critical role. While Piezo1 expression was reported in nonneuronal tissues in the cardiovascular system and Piezo2 expression was confirmed in a variety of sensory neurons.
Work published in nature communications by Rode et al., in 2017, showed that Piezo1 plays a crucial role in physical activity induced blood pressure changes. Transduction of mechanically activated cationic currents by the peizo1 ion channel in the endothelial cell membranes has been reported. See the video for the proposed mechanical activation model of a Piezo1 ion channel, based on Ge et al. 2015 (3D Molecular mechanics).
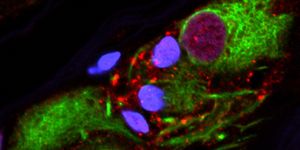
Wei-Zheng Zeng and colleagues have recently published in Science confirming that Piezo1 and Piezo2 are the ion channels responsible for baroreceptor reflex mechanotransduction. The authors studied the expression of these ion channels in the mice sensory neurons of nodose and petrosal ganglion, centers that relay the blood pressure changes to higher cortical structures. By retrograde labeling, the carotid sensory neurons and tracing them to the ganglia, a similar number of cells expressed piezo1 and piezo2 with a small fraction expression were confirmed. The image below shows the anatomy of arterial baroreceptors.

A dose-dependent vasoconstrictor drug-induced changes in BP was used to confirm the ion channels role in baroreceptor reflex from knock out mice models. Vasoconstriction induced a reduction in heart rate, and baroreflex sensitivity was not seen in the double channel knockout mice with a significant increase in the systolic BP when compared to wild-type animal response. Additionally, the aortic depressor nerve activity measured in the double knockout mice also showed no changes when compared to wild-type mice. Monitoring the knockout animal's overtime also showed that daily physical activity significant increase in mean arterial pressure and minimal increase in heart rate. Combined with the blood pressure variability seen overtime in the knockout mice, these observations mimics the symptoms of hypertension.
Zeng et al. also studied the Piezo2 channel roles in activating baroreflex via optogenetic mice models. Light activation of both aortic baroreceptors in the superior laryngeal nerve branch and carotid baroreceptors in the carotid sinus region showed an immediate decrease in both blood pressure and heart rate confirmed the expected efferent sympathetic inhibition following baroreceptor activation. Further blocking this activation by β-adrenergic receptor blocker indicated that inhibition of cardiac sympathetic nerve activity mediates bradycardia reflex activity.
Knowing the key players in the blood pressure neuro-signal communication will allow for research into alternative treatment strategies for cardiovascular ailments. While development of piezo channel agonists may not be an ideal direction of drug development given the broad functional role of these mechanical ion channels, exploring the piezo channel alleles in the context of cardiovascular diseases and targeting them might provide the information.
Sources: Science, Mechanobiology Institute, Singapore