Can Medicine Prevent Cisplatin-associated Hearing Loss for Pediatric Cancer Patients?
Cisplatin is a chemotherapy drug used for pediatric liver cancer and other adult cancers. It has been widely successful in treatment of liver cancer but has the unfortunate effect of causing hearing loss in a great percentage of children treated. Children are living longer after cancer diagnosis; reports indicate that nearly 80% have a five year or more survival rate with many even being considered cured. Their development and interaction for the remainder of their life is dramatically affected by hearing loss. It is reported by the National Cancer Institute that more than 50% of children who use Cisplatin have significant and permanent hearing loss. In adults, there is an estimated range of individuals who report hearing loss after exposure to Cisplatin. For the kids affected, their language development, social interaction, and academic progress.
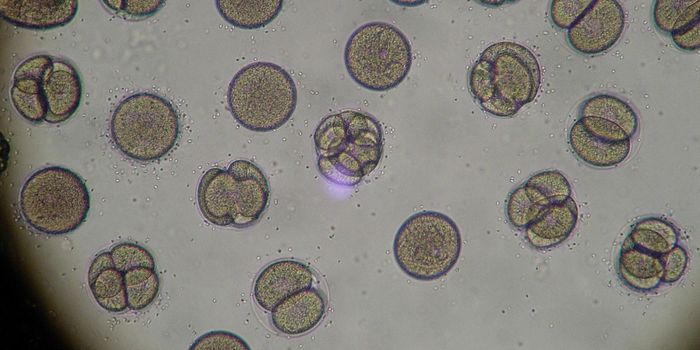
Earlier this year, a study published in Nature Communications looked at the potential cause of Cisplatin’s negative auditory side effect and found that months after treatment, mice and humans had cisplatin molecules remaining in the cochlea, which is the body’s main part of the ear involved with hearing. The group examined many organs for cisplatin residuals and found that most were able to eliminate it days or up to a week after treatment. One researcher indicated that this particular mechanism for hearing loss is not sudden. It is gradual over time and considered a late effect of cancer therapy. Researchers outlined the importance of tracking these cancer patients, especially children, over very long periods of time to monitor their hearing for changes. One grave concern for children is that they may not recognize the change in their hearing until it is so far down the path to significant and permanent loss and may be manifested by poor attention or grades in school or even a behavior problem. Intervention is critical.
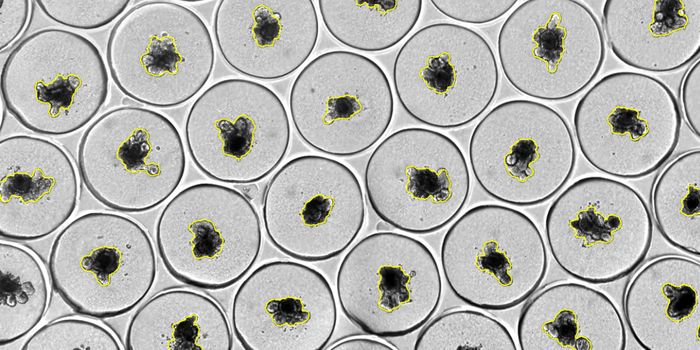
Researchers, like the group working on the mechanism of action in cisplatin associated hearing loss, are working to find methods to block Cisplatin from entering the inner ear through close examination of the cellular mechanism of cisplatin uptake or absorption. The group found that the platinum molecules in cisplatin gather in an area called the stria vascularis, within the cochlea, whose cells modulate the fluid levels that maintain the very sensitive sensory hair cells critical to the process of hearing.
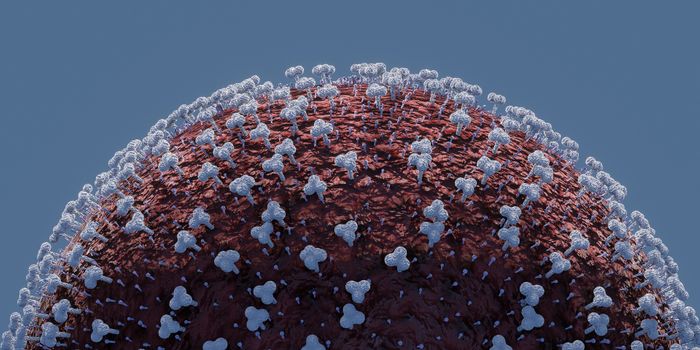
In a recent news release by the National Cancer Institute earlier this month, and a publication in Lancet Oncology, a drug called sodium thiosulfate has been found to potentially prevent the hearing loss generated by cisplatin. Sodium thiosulfate is a chemical used to treat cyanide poisoning and has been used as an anti-viral. It is considered an antioxidant that binds free radicals. These are suspected to be the method for cisplatin residual damage to hair cells of the inner ear. A recently completed phase 3 multicenter, randomized, clinical trial by the Children’s Oncology Group and the National Cancer Institute (NCT00716976) using sodium thiosulfate intravenously after patient cisplatin therapy infusion. Children ages 1-18 could participate and there were dramatic differences in hearing loss identified. From the placebo group, 31 of 55 (56.4%) participants had measured hearing loss; in the intervention group receiving sodium thiosulfate, 14 of 49 (28.5%) participants had measured hearing loss at the primary endpoint of the study and intervention, approximately 4 weeks after final cisplatin dose. There were no serious adverse events associated with sodium thiosulfate use throughout the study. Further study is warranted but this information provides optimism for families and patients who are affected by this long term, and potentially devastating, side effect in their fight against cancer.
Sources: National Cancer Institute, Nature Communications, NIH Open Chemisty Database, Lancet Oncology