Pelvic Radiotherapy Induces Long-Term Inflammation in Cancer Survivors
Radiotherapy (also called radiation therapy), a commonly used cancer treatment that uses high-energy radiation, can effectively eliminate or shrink various types of tumors. While radiotherapy benefits many cancer patients, the associated side effects can hinder cancer survivors' quality of life and overall health.
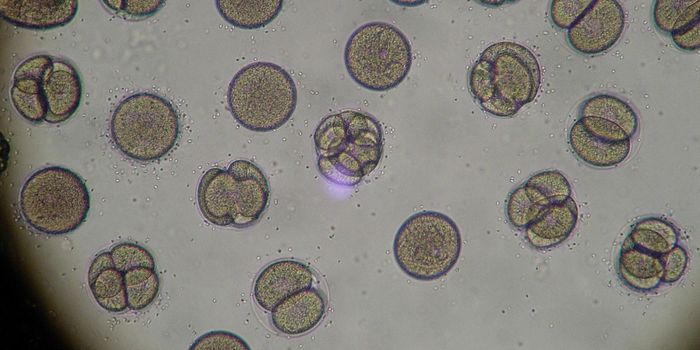
When a patient receives radiation treatments, the radiation damages the DNA. If the DNA damage becomes severe enough, the cancer cell will not recover and will stop dividing and die. Unfortunately, the exact mechanisms by which radiation elicits cancer cell death can cause similar damage in nearby healthy cells, leading to significant toxicities in some cases.
Many malignancies that develop in the pelvic region, including urinary and rectal cancers, are susceptible to pelvic radiotherapy. Some patients receiving pelvic radiotherapy develop debilitating bowel symptoms, including intestinal inflammation. Doctors do not fully understand these clinical challenges despite the common occurrence of bowel symptoms following pelvic radiotherapy. A better understanding of the link between radiation and bowel damage could help doctors manage cancer treatment more optimally, enhancing survivorship.
A team of researchers initiated a study investigating how radiation induces bowel symptoms and recently published their findings in eBioMedicine. Specifically, the researchers wondered how long intestinal tissue remains inflamed after radiotherapy.
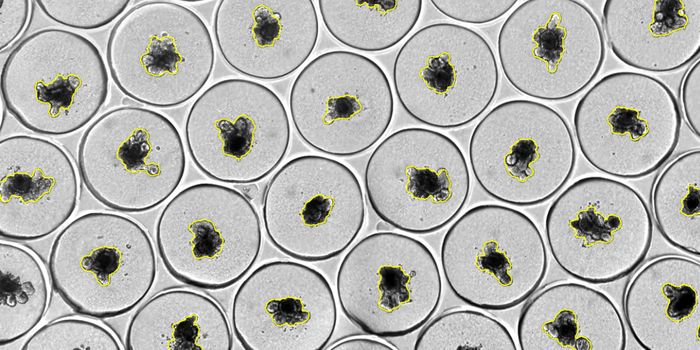
The researchers recruited patients with gynecological, urinary, rectal, and anal cancers who received pelvic radiation. The study enrolled 24 cancer survivors who had received treatment between two- and 20- years post-treatment, and each participant provided a biopsy of mucosal tissue. In addition, four patients who did not receive radiation provided control biopsies.
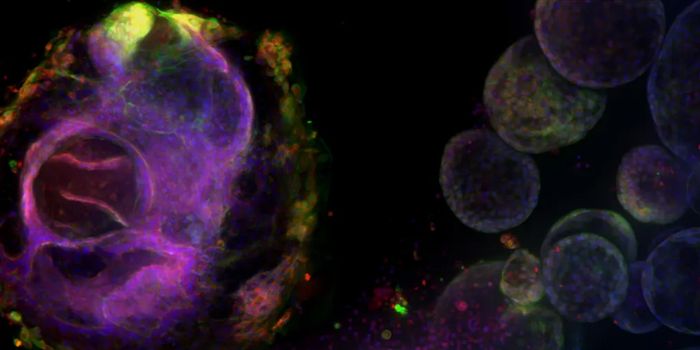
The study revealed 942 proteins expressed differently in mucosal tissue exposed to high-dose compared to low-dose radiation. The tissue exposed to high-dose radiation exhibited low-grade inflammation, indicating immune activity. In particular, the study noted high activity of neutrophils , immune cells that can kill infection-causing bacteria and activate the activity of other immune cells in the body. Notably, acute inflammation and enhanced neutrophil activity occurred as long as 20 years after completing radiotherapy.
The authors conclude pelvic radiotherapy induces acute intestinal inflammation that does not progress to chronic inflammation. Thus, further investigation into strategies aimed at mitigating low-grade inflammation could aid in treating cancer survivors who received pelvic radiation.