Everyone knows sleep is important. Getting a good night’s sleep resets your brain, allows for efficient cell repair and aids in effective digestion. Interruptions in sleep/wake cycles, otherwise known as the circadian rhythm, have long been thought to contribute to cancer progression due to changes at the cell and tissue level.
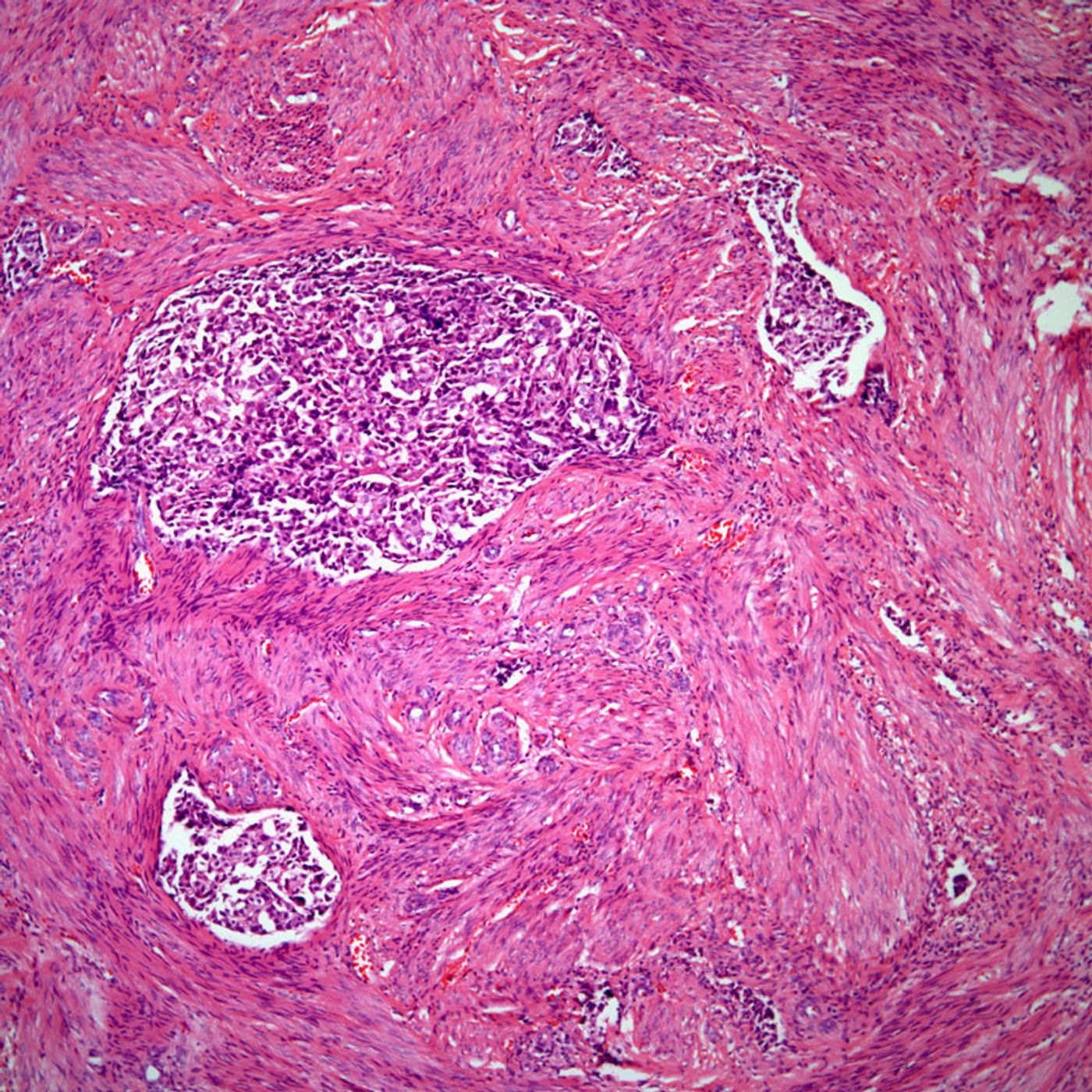
Scientists at the National Cancer Institute have recently discovered that one of the circadian rhythm genes can specifically affect breast cancer metastasis. Breast cancer is one of the most common diagnoses in women in the United States, and breast cancer metastasis is the second leading cause of death in women. It is commonly known that the primary tumor is not what causes the high mortality rates in cancer; it is the metastasis of that tumor to other body parts. Metastasis can be hard to contain, and depending on the tumor type, might not have targeted therapies to treat.
To complicate things even further, there are several different subtypes of malignancy that can affect tumor progression and treatment options. Two subtypes of breast cancer, ER+ (estrogen receptor-positive) and HER+ (human epidermal growth factor-positive), have targeted therapies specifically developed to these types of tumors even after they have disseminated throughout the body. These treatments target the tumor cells directly and negate the need for general therapies such as chemotherapy.
However, ER- and HER- tumor types do not respond well to these therapies and have a higher chance of metastasis and poor survival prognosis. A better understanding of the biology and genetics behind these ER- and HER- tumors would provide the basis for new targeted therapies and clinical treatments to improve the outcome of diagnosis and malignancy in these patients.
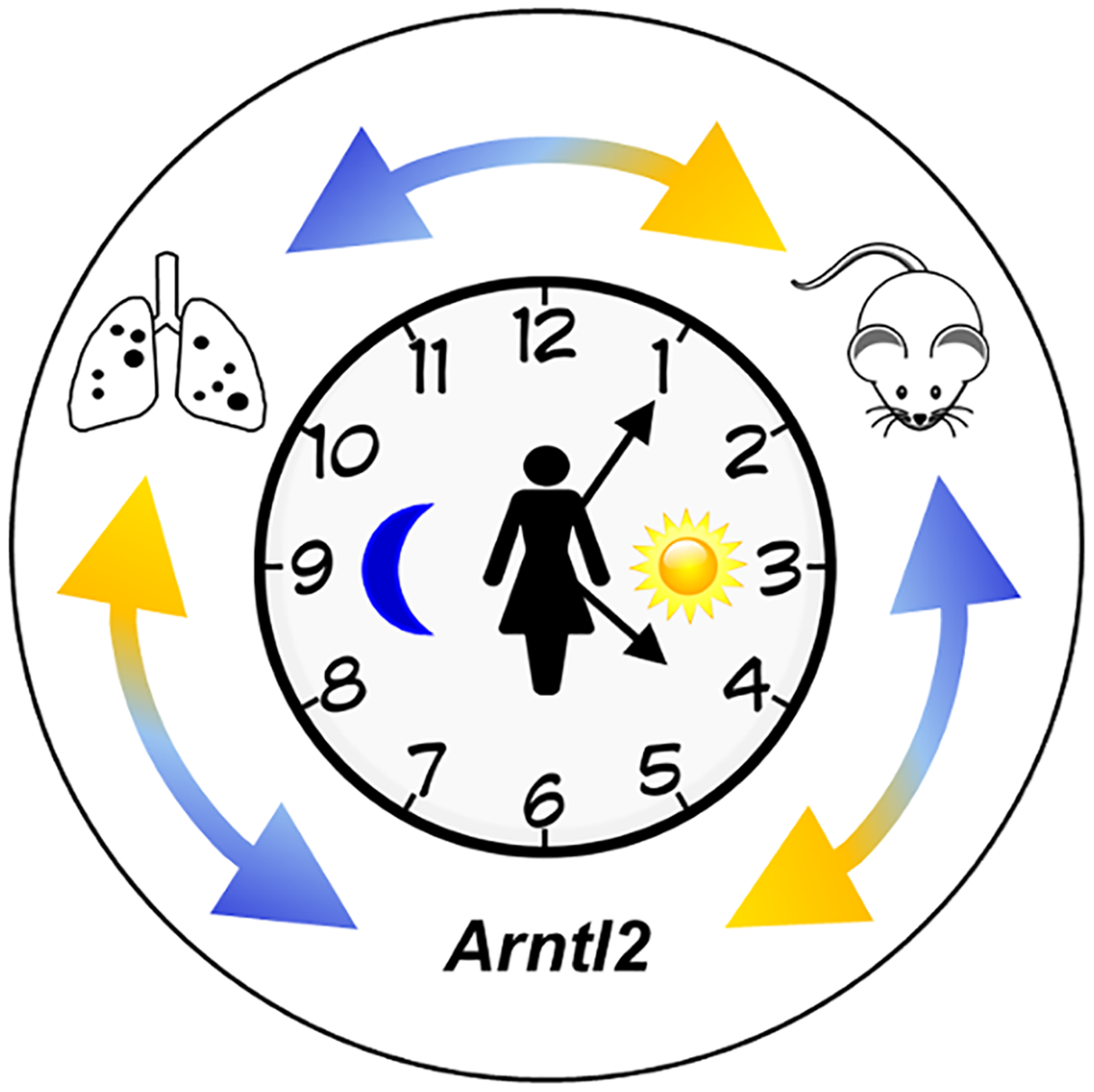
Studying crosses of genetically engineered mice with highly metastatic mammary tumors with those containing low frequency metastatic tumors provided gene signatures consistent with the ER- cancer subtype and led to the identification of Arntl2, a known circadian rhythm gene, as a metastatic susceptibility gene. Kent Hunter, one of the primary authors of the study and Senior Investigator at NCI, notes that this association suggests circadian rhythm plays a role in both the cause and progression of this very aggressive form of breast cancer.
Based on mapping data from the cross, researchers genotyped an area that highlighted the Arntl2 gene as a primary cause for progressive metastasis in the mice and related cell lines. Further knockout experiments and association-based patient cohort studies were done to validate the Arntl2 gene as a causative gene to metastatic-specific cancer progression in the ER- subtype.
This study, published in
PLOS Genetics, sheds light on metastasis and the many factors that enable a primary tumor to spread. Metastasis is a complicated process influenced by many factors, such as obtaining invasive and migratory abilities, gaining entry into the lymphatic system, and colonization of cells in a new environment. Given the different factors that go into cancer progression, it has become evident that there are several outside influencers and biological processes that can positively or negatively affect tumor progression.
Circadian rhythm disruption has been indicated in previous studies to increase breast cancer risk and survival rates based on epidemiological and gene expression studies. However, there have not been any causal effects shown until now. Hunter and team were able to prove that Arntl2 has a direct effect on the metastasis of ER- breast cancer. These findings provide a genetic basis for inherited susceptibility of cancer metastasis and emphasize the potential of incorporating behavioral adjustments such as more sleep and sustained sleep/wake cycles into cancer treatment.
Sources:
PLOS Genetics,
NCI,
Reuters,
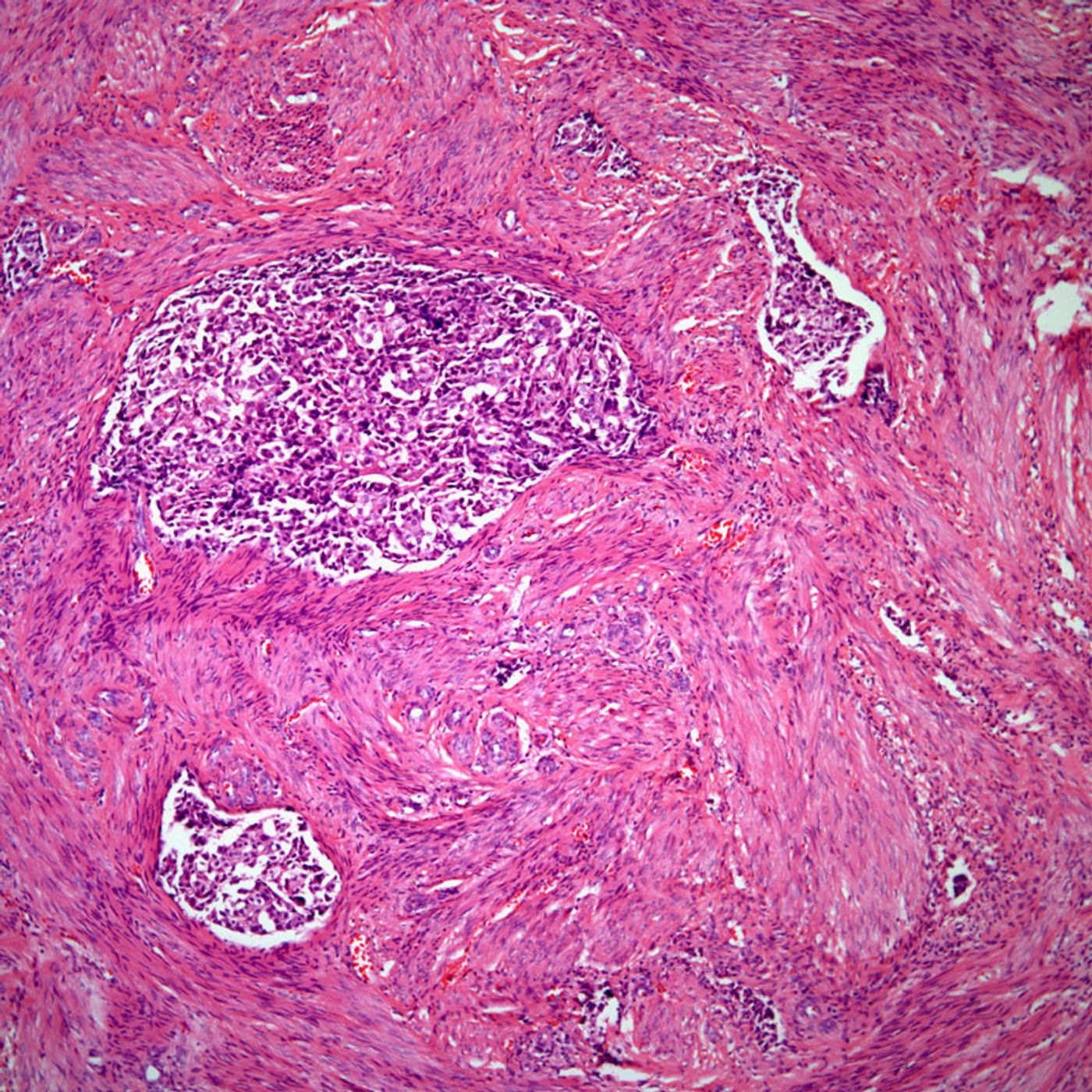
Arntl2 Image