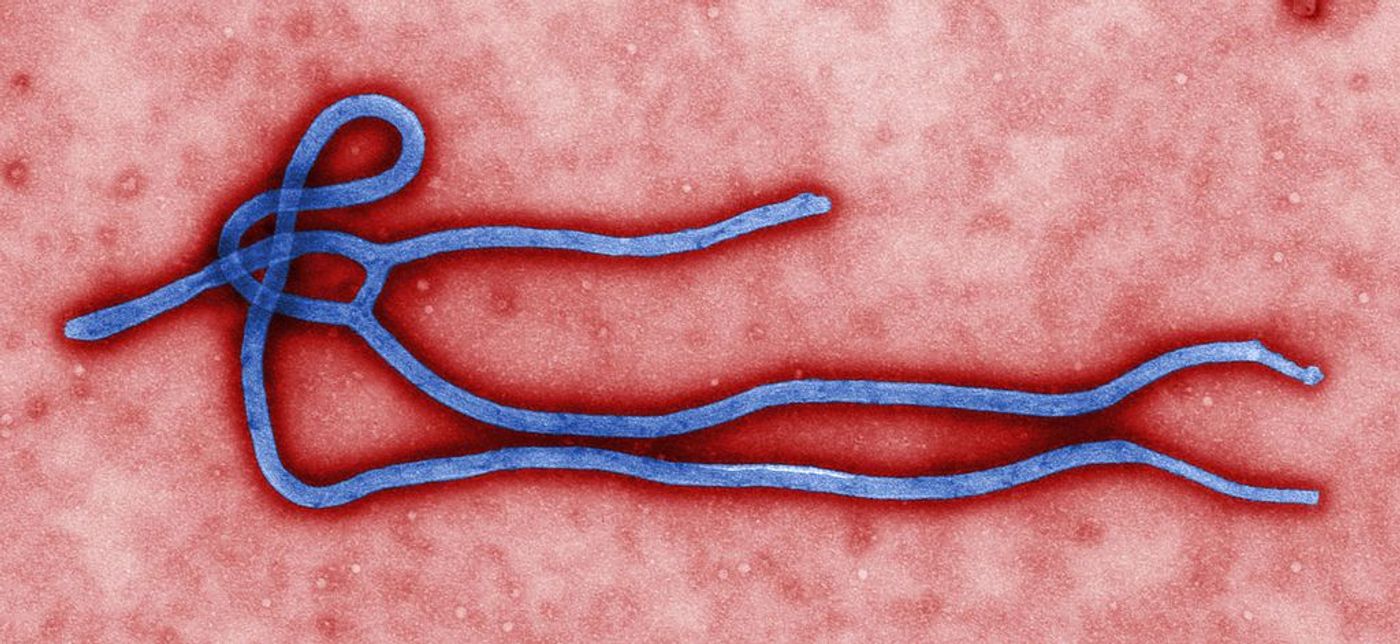
T Cell Response to Ebola Virus Proteins
Ebola virus disease (EVD), first identified in 1976, is a severe illness with a fatality rate around 50%, with rates ranging from 25-90% for specific outbreaks. Most recently the ninth outbreak of Ebola in the Democratic Republic of the Congo ended on July 24th, 2018. No cure currently exists, but experimental Ebola vaccines have proved protective against the virus in major trials lead by the World Health Organization. A recent study from scientists at Scripps Research Institute offers guidance on effective Ebola vaccines after studying T cells in Ebola survivors.
Ebola virus can be transmitted through symptomatic individuals’ blood or body fluids, contaminated objects (needles and syringes), and infected fruit bats or nonhuman primates. Even after an infection has cleared the virus can remain in certain fluids such as semen and breast milk, allowing for continued transmission. Symptoms can include fever, headache, fatigue, diarrhea, vomiting, and hemorrhaging. The current treatment for Ebola includes treating symptoms as they appear, often involving intravenous fluids and electrolytes, oxygen therapy, blood pressure medication, and treating secondary infections. No antiviral drugs exist that are approved by the U.S. Food and Drug Administration, but those currently being developed stop the virus from creating copies of itself in the body.
T cells play an important role in clearing virus during acute infection, but little is known about the specific response of T cells during Ebola infection. A study from Scripps Research Institute examined CD8+ T cells, also known as killer T cells, in 32 Sierra Leonean survivors of the 2013-2016 epidemic. These killer T cells are designed to destroy infected cells that are producing the Ebola virus. Blood samples were analyzed to characterize the total killer T cell response to Ebola virus proteins in the survivors. Cells infected by the virus express eight different proteins, encoded by the Ebola virus’s genetic material, on the cell surfaces. Previous studies have suggested the Ebola virus’s glycoproteins are the main target of an effective immune response, so most Ebola vaccines are designed with the Ebola glycoprotein.
To test the interaction of killer T cells with these proteins, scientists cut the viral proteins into peptides. These small pieces of the proteins can complex with proteins unique for each individual, called human leukocyte antigen (HLA). An HLA/viral peptide complex is formed and transported from inside the infected cell to the outer surface. When this complex presents on the surface, it can be recognized by killer T cells which will trigger the destruction of the infected cell. Of these eight proteins seven were tested, and the research team found that 96% of the survivors made killer T cells that responded to the nucleoprotein of the Ebola virus. Comparatively, only 38% of the survivors responded to the virus’s two glycoproteins. In addition, the study revealed 34 new sites that killer T cells specifically target on Ebola virus proteins, which will help elucidate how the immune system targets the virus.
Future work will study samples from people who may have been infected with the Ebola virus but remained asymptomatic, such as family members of epidemic victims. Regarding Ebola vaccine development Dr. Michael B. Oldstone, senior author of the study, said: "Our study of the immune response in Ebola survivors, suggests that a vaccine targeting not only the glycoprotein but Ebola's nucleoprotein would likely be more effective than the current vaccines that only express the glycoprotein."
To read this study click here. To learn more about Ebola watch the video below!
Center for Disease Control, World Health Organization