The History of Vaccines
Everyone worldwide is sitting with anticipation, waiting for the right vaccine candidate for the coronavirus outbreak, hoping that it will end this pandemic nightmare. The same happens anytime a new disease rises to the surface and spread to many countries or all over the world.
Vaccines are always one of the best solutions to end a widespread infectious disease, but who invented the idea of vaccines and how long ago? what are the different types of vaccines? have scientists managed to end a pandemic before using vaccines?. Let's dive into the history of vaccines.
The English doctor Edward Jenner is considered the founder of vaccinology in 1796, although the concept of vaccinology had been practiced before in China and Europe.
Jenner was present in the times of widespread smallpox infection. At that time, it was known between farmers that whoever gets infected with cowpox, another viral skin infection that causes pus-filled lesions on the skin, doesn't get infected with smallpox. He used his analytical and scientifically driven mind to observe this fact and took pus from a cowpox lesion on one of the milkmaid's hands, then injected a little boy with it. Several weeks later, he inoculated two sites on this boy's arm with smallpox, and the results were marvelous! The boy didn't get infected with smallpox.
This great observation was the basis for developing the first known vaccine for smallpox by Jenner and the foundation for the science of modern vaccinology.
The word vaccine had referred only to cowpox inoculations for smallpox until the French scientist Pasteur developed another vaccine for rabies in the 1800s, which he called rabies vaccine. Pasteur was studying chicken cholera, a bacterial disease that causes diarrhea, trying to develop a vaccine for cholera. He cultured the bacteria in the lab then injected the chickens with it; however, many chickens died after the procedure.
He continued his research by culturing more bacteria in the lab; however, by accident, he used old cultures of bacteria that have been exposed to air and inoculated them into chickens. Surprisingly the chickens showed mild illness which caught his attention, afterward, he inoculated freshly cultured bacteria into the chickens and the results were astonishing, the chickens didn't develop any symptoms. He made the conclusion that shaped the meaning of a vaccine until today, that the weekend form of the bacteria didn't kill the chickens but allowed their immune systems to practice fighting the infection, and since immune cells have memory and can recognize the same infection when reexposed to it, the second time chickens were exposed to the bacteria, their immunity worked and fought it successfully.
A vaccine is an attenuated or weakened form of a microorganism injected into the host to allow immunity to recognize the infection and fight it.
Pasteur tried this with rabies, but it was different since rabies is caused by a virus, not a bacteria, which was not known at the time; therefore, he couldn't culture it in the lab. He tried a different approach and passed the virus several times in another species, rabbits, which resulted in weakening the virus and protecting dogs against it, which encouraged him to try it in humans; he succeeded and became a hero.
The explanation of what happened is, viruses are highly mutating. By a serial passing them into a different host species, they mutate and adapt to the new host while becoming less adapting to their original host; they become attenuated with less virulence making them suited to be used as a vaccine.
Since then, many vaccines were developed for different infectious diseases helping in ending some endemics as smallpox, bird flu, influenza outbreaks and also helped in the reduction in the number of cases for diseases as polio vaccine for poliomyelitis and vaccines for measles and chickenpox.
Do all vaccines are the same? Do immune systems respond in the same way to all? The answer is no, and there are four main types of vaccines depending on the technology used for developing the vaccine, the immune system's response, and who gets vaccinated.
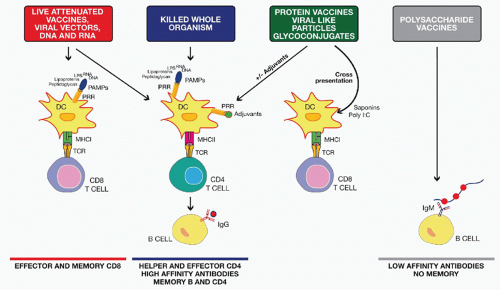
Mode of action of different classes of vaccines. Credit: Oncohema Key
Live-attenuated vaccines, Inactivated vaccines, Subunit or conjugate vaccines, and Toxoid vaccines.
Live vaccines use attenuated or weakened versions of the microorganism, not strong enough to cause severe damage but have enough information to induce an immune response. Some examples are vaccines against measles, chickenpox, smallpox, and rotavirus.
Inactivated vaccines use a dead version of the microorganism causing the disease; this is why they don't provide long-term immunity as live vaccines and needs several booster shots. Some examples are hepatitis A, polio, and rabies vaccines.
Subunit and conjugate vaccines use a particular part of the microorganism as its protein, capsule, or sugar. They provide strong immunity against infections since they are targeted against a specific part of the microorganism. Some examples are hepatitis B, HBV, whooping cough, and shingles vaccines.
Toxoid vaccines use a toxin made by the microorganism that causes the disease. It targets the toxin instead of the whole microorganism. Some examples are diphtheria and tetanus vaccines.
Recently, in response to the COVID-19 pandemic, we have heard about mRNA vaccines, they use mRNA sequence that carries the information for the production of a specific part of the microorganism to induce an immune response against that part. mRNA vaccines are cheaper and faster than traditional vaccines. Hopefully, they will help in ending the COVID-19 pandemic.
Sources: The Immunisation Advisory Center, Health Affairs, Vaccines.gov, VBI Vaccines, History of Vaccines, University of Cambridge








