Combination Treatment Targets Previously Undetected Tumor Cells
Chemotherapy has long been the gold standard for cancer treatment since its inception in the 1950s. Chemotherapy is a treatment that uses a chemical to target and kill cancer cells. More specifically, these chemicals are responsible for dysregulating reproductive mechanisms in cancer cells, so they cannot multiply. However, lack of treatment efficacy, tumor specificity, and increased toxicity has driven scientists to investigate other therapeutic alternatives. Since the 2000s advancements in immunotherapy have provided more effective options compared to chemotherapy alone. It is becoming more common to pair chemotherapy with immunotherapy to hit the tumor in two waves for “complete” eradication.
Immunotherapy is a broad term referring to therapeutic treatments that use the immune system to recognize and attack the tumor. It has become increasingly well known that tumors remain undetected by expressing specific molecules and using various mechanisms that divert immune cells. A common subtype of immunotherapy includes immune checkpoint inhibitors (ICI). In this therapy molecules on tumor cells or others present a marker to inactivate immune T cells from attacking the infected cell. One example of an effective ICI includes anti-PD-1 therapy. In this treatment the drug blocks the interaction of the molecule on tumor cells known as programmed cell death-ligand 1 (PD-L1) and its receptor, programmed cell death- 1 (PD-1) on T cells. The interruption of this binding site allows T cells to then recognize the tumor and kill it by triggering cell death signals. Unfortunately, tumors can still evade the immune system by becoming senescent or fail to reproduce. The immune system scarcely detects senescent cancer cells, and this can result in slow cancer regrowth. Many researchers are investigating how to combat this senescent characteristic of tumor cells.
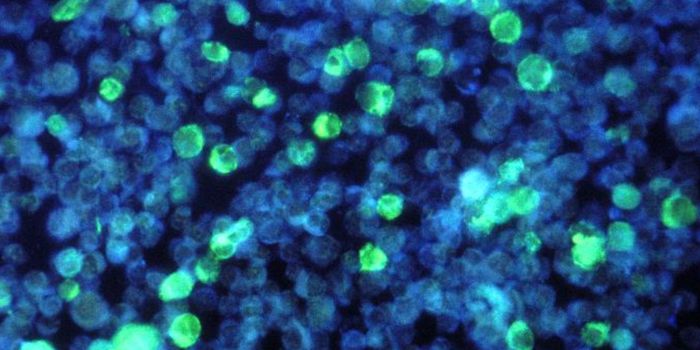
A recent article published in Nature Cancer by Dr. Manuel Serrano and his team have investigated the combination of chemotherapy and immunotherapy to improve cancer treatment efficacy. Serrano is a Group Leader at the Institute for Research in Biomedicine (IRB) Barcelona and has worked to overcome senescent tumor cells. Serrano and others used animal models for three different cancers (melanoma, pancreatic, and breast) to discover that cancer cells become senescent after chemotherapy by activating the PD-L2 protein, a lesser-known ligand of PD-1. PD-L2 was recently shown to be an upregulated marker in senescent tumor cells. The group of researchers found that PD-L2 not only prevents the immune system to attack the tumor directly, but also recruits immune suppressive cells to create a tumor microenvironment favorable for tumor progression. Additionally, tumor cells lacking PD-L2 are quickly recognized and kill by the immune system. To further analyze this phenomenon, researchers blocked PD-L2 and found increased tumor lysis after chemotherapy treatment. These findings demonstrate a synergistic effect between chemotherapy and PD-L2 immunotherapy. In the regimen Serrano and his team introduce, chemotherapy kills most of the cells, but those that go undetected due to their retained senescence are then killed by PD-L2 blockade.
Serrano and others mechanistically demonstrate how to overcome senescent tumor cells after chemotherapy. Through adjuvant or additional immunotherapy after chemotherapy, researchers were able to significantly reduce tumor growth. This opens the door for a novel regimen with PD-L2 that effectively kills the tumor. Overall, this new treatment strategy provides the potential to enhance treatment efficacy in various cancer types and improve patient survival.