Some cells in the immune system are for constantly pumping out antibodies during an infection, while others are saved for later should the same pathogen strike again. In a new study from the Emory Vaccine Center and Stanford’s Department of Pathology, scientists investigated how the immune system differentiates between the two types of cells, in order to adapt a similar process to the development of more effective vaccines.
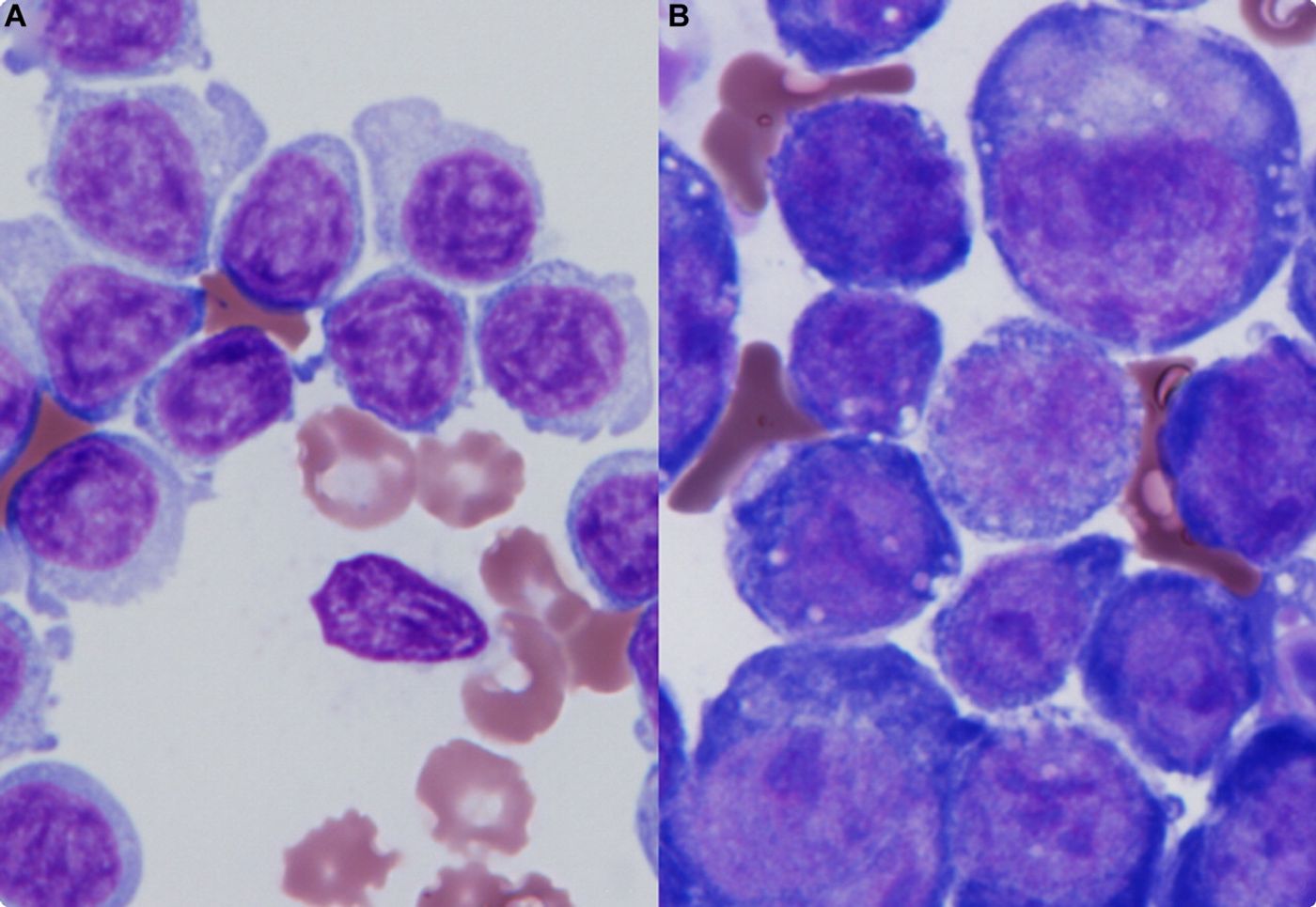
Plasmablasts are responsible for immediate antibody production when a pathogen invades the body. Activated B cells, the immune cells that precede memory B cells, don’t secrete antibodies spontaneously like plasmablasts do. However, they can be stimulated to secrete different antibodies according to the content of their DNA. In their recent study published in the journal
Nature Immunology, researchers tracked the path of B cells during an immune response by following their DNA patterns.
The team of scientists studied the activity of activated B cells after influenza vaccination, after influenza infection, and during Ebola virus infection. Why Ebola? “Ebola virus infection represents a situation when the patients’ bodies were encountering something they’ve never seen before,” said lead author Ali Ellebedy, PhD. “In contrast, during both influenza vaccination and infection, the immune system generally is relying on recall.”
One week after study participants were immunized for influenza, both flu-specific plasmablasts and flu-specific activated B cells were detected in their blood. However, two weeks after the immunization, the plasmablasts had completely disappeared from the blood, while the activated B cell cells were still proliferating.
Months after the immunization, activated B cells had completed the transition into resting memory B cells, giving scientists the full picture of how memory cells are produced.
Additionally, they saw a similar trend in Ebola patients with a progressing infection: as the plasmablast count decreased in the blood, the activated B cell count increased.
With more insight into how antibody-producing cells diminish over time, researchers might make some changes to the way vaccines are created.
“It is still worthwhile to encourage the immune system to make a greater quantity of antibodies, even if their quality does not rise appreciably, and the value of vaccination may be greater when the flu vaccine strains are not identical to those used in previous seasons’ vaccines,” Ellebedy said.
Source:
Emory Health Sciences
Image: Blood Journal