Crossing the Blood-Brain Barrier: Improving Experimental Models to Study Drug Delivery
The blood-brain barrier (BBB) describes the complex vasculature network that delivers oxygen and nutrients to the brain. The blood vessels that make up the BBB regulate the flow of biological molecules and cells between the bloodstream and the brain.
While the BBB serves a crucial biological function in protecting the brain from invasion by pathogens and toxins, it can also restrict drugs from entering the brain. This can considerably diminish the effects of highly specialized cancer therapies. Therefore, research concentrating on allowing beneficial molecules to pass the BBB could significantly enhance our ability to treat cancer.
Not all biomedical research can be performed in human volunteers, so researchers often use animals, referred to as in vivo models, to mimic human pathology and aid in the development of new therapies. However, studying the BBB in animal models presents challenges preventing accurate translation into the clinical setting. This has resulted in a substantial need to develop in vitro methods that are representative of human physiology to explore methods to efficiently deliver cancer therapies across the BBB. In vitro cancer models are essential for cancer research and are necessary to advance drug discovery and development. They are used to help researchers understand how cells and other biological mediators interact. Such models can be used to help explore therapeutic strategies considering the personalized complexities of an individual patient’s cancer.
A study published today in Nature Protocols describes a novel in vitro technique to model the BBB within a microfluidics system. The protocol improves upon current in vitro BBB techniques which only utilize a single layer of cells that fail to recapitulate the three-dimensional organization of the brain vasculature.
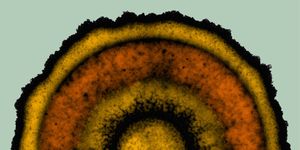
The new methodology incorporates the three major cell types present within the BBB: endothelial cells (ECs - the cells which line the blood vessels), pericytes (PCs - cells located near ECs in the blood vessels), and astrocytes (ACs - cells that secrete proteins needed for BBB composition). The ECs, PCs, and ACs are embedded in a three-dimensional gel matrix in a microfluidic device, a laboratory instrument that analyzes bodily fluids, including cellular components, on a microchip.
Once embedded into the matrix, the cells interact and form a replica of the human BBB. Notably, the researchers demonstrate that the ECs from their in vitro BBB model express a similar gene profile as observed human brain ECs. Further, the permeability of molecules in this BBB model is comparable to that measured in vivo.
The new article describes the novel method of developing this clinically relevant in vitro BBB model. The authors also provide instructions on measuring permeability when using this system. The detailed protocol will enable other researchers to utilize this model to investigate methods of improving drug delivery across the BBB and develop new anti-cancer drugs. Author Dr. Giovanni Offeddu spoke to Labroots, highlighting the importance of this model. Offeddu stated, “the brain vascular models and methodologies that we developed can help accelerate the development of medicines for neurological diseases that currently have no cure.”
Tumor vasculature is an important factor for the development and progression of most types of cancers, not just those that involve the brain and central nervous system. Like the BBB, blood vessels surrounding cancers outside the central nervous system deliver nutrients needed for tumor growth and expansion. Many cancers initiate a biological process called angiogenesis which promotes the development of new blood vessels to aid in cancer progression and spread. Cancer-associated angiogenesis is characterized by the formation of disorganized and dysfunctional vasculature. Therefore, the unique vascular networks that grow around tumors allow the delivery of growth factors and nutrients to cancer but restrict the delivery of anti-cancer drugs.
The formation of excess connective tissue around a breast tumor, known as breast cancer desmoplasia, is often associated with a poor prognosis. These types of breast cancer diagnoses are difficult to treat due, in part, to the diversity of the vasculature that forms around the tumor. Because there is little consistency between patients, determining a standard treatment has proven challenging. The same research group has applied their technique to another study relevant to improving breast cancer treatment. A pre-print of this manuscript, released through bioRxiv, has used personalized in vitro models to explore ways of improving drug delivery to breast cancer.
The study used a unique in vitro tool, called tumoroids, generated from cells and tissue derived from breast cancer patients. Under specific in vitro conditions, tumoroids cluster into a three-dimensional orientation that can mimic the breast cancer tumor microenvironment (TME). The tumoroids used for the pre-print study replicated specific aspects of breast cancer, including poorly functioning vascularization that impedes drug delivery to a tumor. This system gave the researchers an innovative strategy to explore methods of delivering critical therapeutics directly to cancerous tissue.
Breast cancer is a diverse disease often described based on the receptors present or absent in a specific patient. Doctors typically consider the estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) expression in a patient when determining an appropriate course of treatment. The study also considered these factors, generating tumoroids modeling three specific subsets of breast cancer: ER+/PR+, HER2+, and ER-/PR-/HER2- (often referred to as triple-negative).
The three-dimensional in vivo modeling described above presents a great technique to study the impact of tumor vasculature on drug delivery. Using the tumoroid models, the authors identified several factors which impaired drug delivery to the tumor. The researchers measured high levels of hyaluronic acid around tumor cells and recognized this as one such indicator associated with poor drug delivery. They also noted a reduction in perfusion capacity in the vessels closest to the tumor cells, further impairing drug delivery. Finally, the researchers found that elevated interstitial fluid pressure around the tumoroids prevented effective drug distribution to the cancer cells.
The authors then used the tumoroid models to study how new therapies could address the factors that are negatively associated with drug delivery. Their data suggests two potential therapeutic targets to improve drug distribution into the tumor. One target is the cytokine interleukin 8 (IL8), a pro-inflammatory immune mediator that influences blood vessel formation. The researchers found that treatment with an antibody blocked IL8, prevented upregulation of hyaluronic acid, restored perfusion capacity, and reduced perfusion interstitial fluid pressure.
The study suggests that IL8 could be an effective target to combat the negative impacts of tumor-driven vessel dysfunction. Further investigation of anti-IL8, and other modalities that correct vessel dysfunction, as an anti-cancer therapeutic modality could significantly improve drug distribution into breast tumors.
These studies demonstrate very innovative strategies to model systems that have proven challenging for researchers. The protocols developed by this team of researchers using three-dimensional microfluidic devices have the potential to significantly enhance these areas of research. This work presents practical alternatives to animal models for studying both the BBB and desmoplastic breast cancer. Further, these technologies may be applicable to other cancers and diseases currently lacking appropriate experimental models.
Sources: Cold Spring Harb Perspect Biol, Nature Protocols, Cancer Discovery, bioRxiv, Oncotarget