Compound Shrinks Tumors of Sarcoma Cells
According to a multi-disciplinary study carried out by the University of Illinois, a compound was found to effectively shrink tumors in animal models by targeting receptor proteins on sarcoma cancer cells.
Learn more about sarcoma:
"There's a very poor prognosis with sarcomas. Sarcomas are rare tumors, but they are so heterogeneous that they're very difficult to treat," explained Dipanjan Pan, a professor of bioengineering and in the Carle Illinois College of Medicine and lead author of the study. "The receptor we targeted inside the cancer cells, the orphan nuclear receptor, is a more universal target for the varied sarcomas than markers on the surface of cells. The opportunity is huge, because this receptor is also expressed in other types of solid cancers -- melanoma or liver cancers, for example."
Specifically, the researchers targeted a protein found abundantly in individuals with sarcoma and other cancer cells but present in low concentrations in normal healthy cells—this protein is called the retinoid X receptor (RXR). Most recently, a drug class targeting RXR has been developed. However, the drug was found to be very toxic and comes with limitations. Therefore, researchers were encouraged to look for better compounds that would be most appropriate for targeting RXR in regards to safety and efficacy.
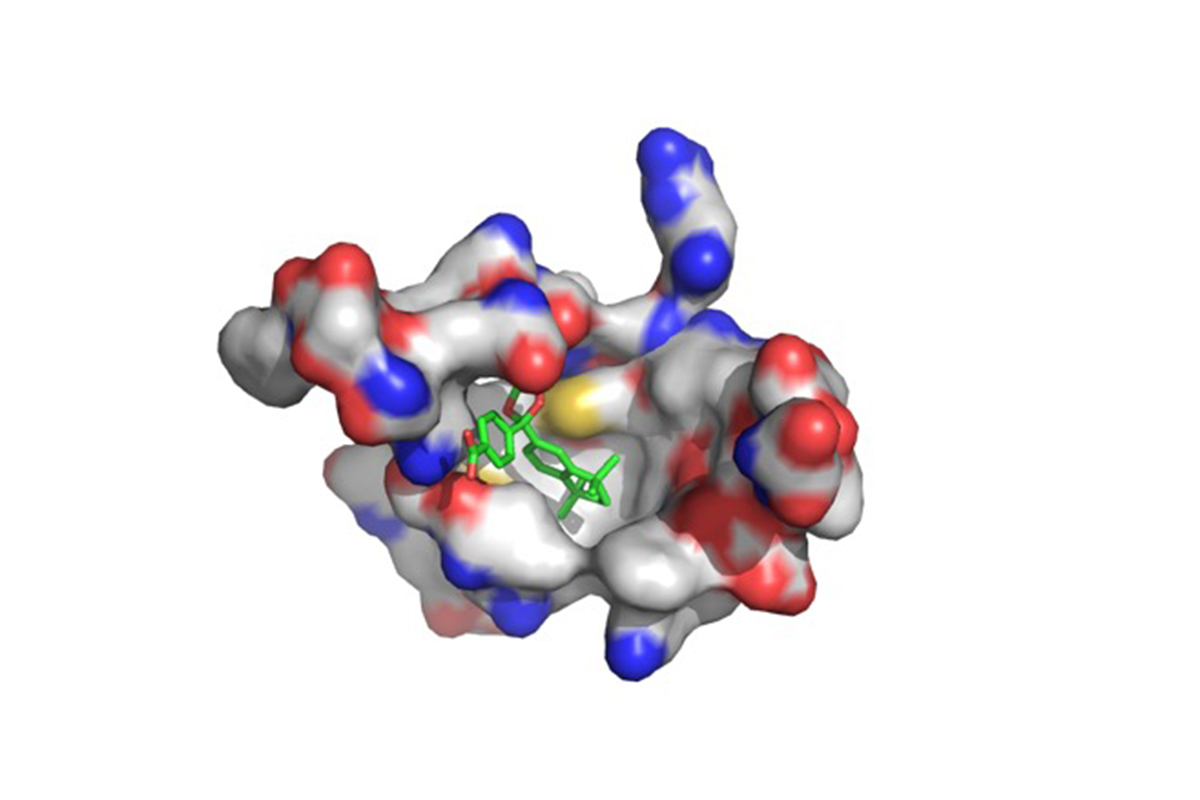
The new compound, shown in green, fits precisely into the active site within the target protein, retinoid X receptor. Image courtesy of Dipanjan Pan via University of Illinois
When the most promising compound was picked out of 20,000 likely candidates, it was synthesized and tested on tissue culture cells. After successful results, the compound was then tested on a sarcoma-pig model. The results, published in Journal of Medicinal Chemistry, shows that tumors successfully shrunk and were less likely to metastasize. No specific toxicity was sobered or measured however, there was some side effects. "We saw that the tumor was shrinking, but that doesn't mean the drug is working the way it's supposed to work," Pan said. "We wanted to make sure that the drug was actively participating in the pathway we intended, and that it wasn't just killing cells because it's toxic.
Source: University of Illinois