Your Personal History with the Flu Impacts How You'll Respond to the Vaccine
Don’t dismiss the seasonal flu vaccine just yet. There may be more to its ineffectiveness than meets the scientific eye - and scientists from the University of Chicago Medical Center are prepared to explain why.
A new phenomenon called “original antigenic sin” describes the previously unexplored impact of an individual’s history of exposure to the flu - via infection or vaccination - on a particular flu vaccine’s effectiveness.
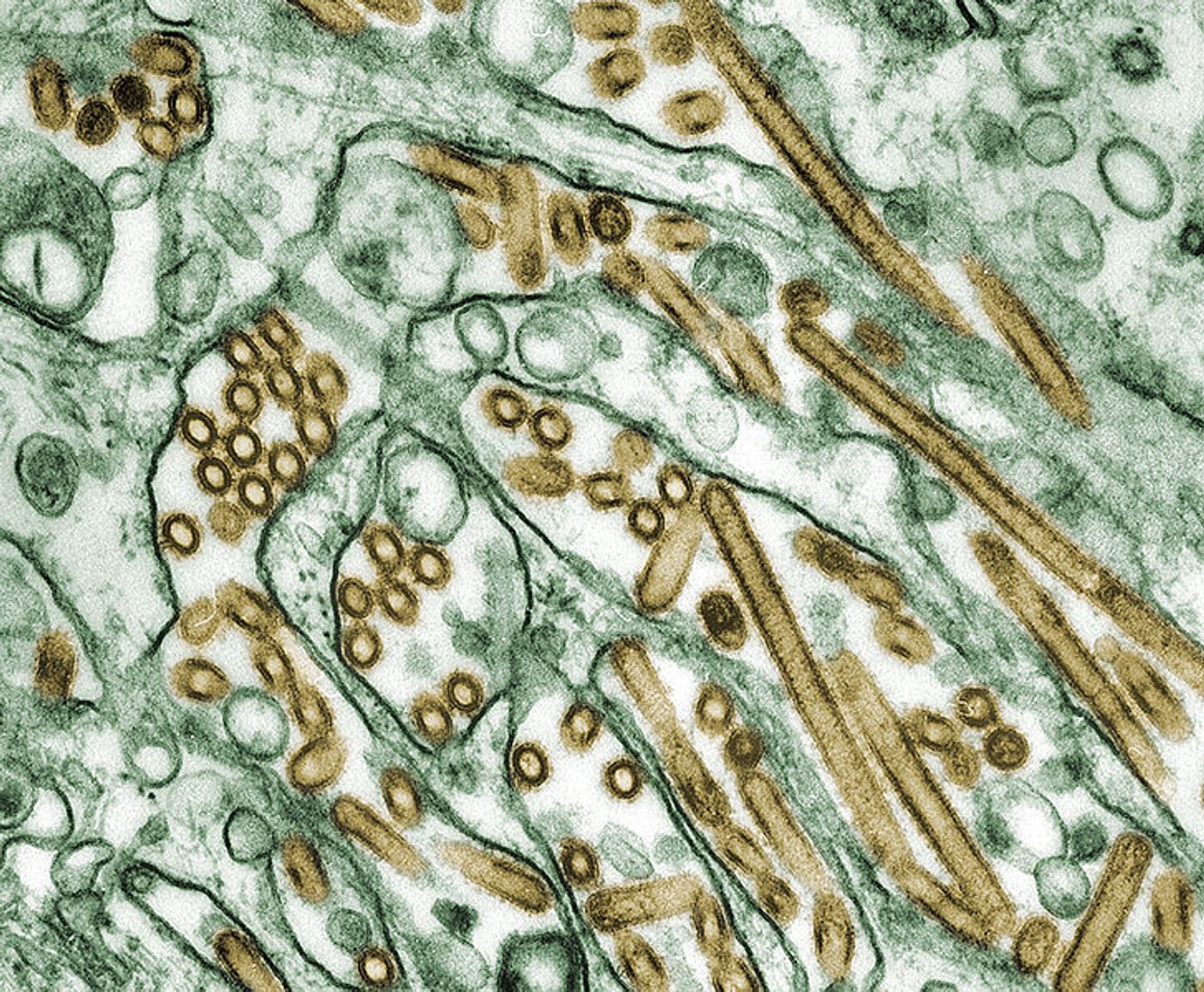
The flu vaccine is developed prior to each upcoming flu season, designed to activate the immune system through antibody production. Antibodies are specifically tuned to recognize the flu strains anticipated by experts to be prominent in the upcoming year. Antibodies bind parts unique to the virus to prevent it from invading human cells. But in 2012 and 2013, the flu vaccine was only effective for 39 percent of people who received the vaccine, and reports of ineffectiveness in the current batch of vaccines abound.
In the past, scientists have explained that ineffective flu vaccines are a natural result of the imperfect process of prediction. Sometimes the strains incorporated into vaccines, predicted to be the most common, simply aren’t as relevant as scientists thought they would be.
Another potential problem is the fact that most flu vaccines are grown in eggs, where the virus can mutate and become different than what scientists intended to protect people from. So even if the experts are correct in their predictions, there’s a chance that the strains will change during development.
While the egg-growing issue has not been rendered irrelevant by the discovery of “original antigenic sin,” the research findings from the University of Chicago Medical Center show this other phenomenon might be more important for explaining vaccine ineffectiveness.
"Egg adaptations have variable effects," explained lead author Sarah Cobey, PhD. "Sometimes they matter and sometimes they don't, but what seems to make the most difference is immune history."
The vaccine given in 2016-2017 is a good example of when changes during egg growth negatively affected the protective abilities of the flu vaccine. Egg-growing changes are also potentially affecting the 2018 vaccine.
“Original antigenic sin” describes a tendency of the immune system to produce antibodies based on its first exposure to the flu - either through an infection or a vaccination. So when a person receives the flu vaccine after years of receiving getting vaccinated and potentially catching the actual virus once or twice, the immune system still relies primarily on the antibodies produced during the first flu exposure. If those antibodies aren’t effective against the circulating strain, then the individual isn’t as protected against infection as they could be.
The 2012-2013 flu vaccine was also believed to be negatively affected by egg changes. When researchers gave the vaccine to ferrets, they exhibited a poor immune response to H3N2, the most prevalent strain that season. But when the vaccine was given to humans, the immune response to the vaccine and to H3N2 strains were virtually the same. How is this possible?
"Imagine influenza viruses are like different makes and models of cars," said Grad. "The ferrets, which hadn't seen influenza before, learned to tell the difference between closely related strains - like telling the difference between a Honda Civic and a Toyota Camry. But people didn't distinguish between them and instead just saw cars."
Going forward, Cobey and her team are investigating “original antigenic sin” further, as well as joining other research teams in experimenting with ways to grow flu vaccines that don’t involve eggs.
"We also need to understand why the vaccine appears to be bad at eliciting responses in some people some of the time,” Cobey said. “Is there really no response, or are we just not looking in the right places?"
The present study was published in the journal Clinical Infectious Diseases.
Sources: Centers for Disease Control and Prevention, University of Chicago Medical Center