Leprosy. We’ve all heard of it, but do you really know what causes it?
What does the word make you think of? A disease that people got a long, long time ago? A super-contagious condition that causes physical deformities? Let’s take a few minutes to debunk some myths surrounding this disease.
Leprosy has affected humans throughout history and continues to do so even today. In fact, someone is diagnosed with leprosy every two minutes, and 106 countries reported new cases of leprosy in 2015! The disease likely originated in Africa and followed humans across the globe as they migrated - it probably reached the West within the last 500 years.
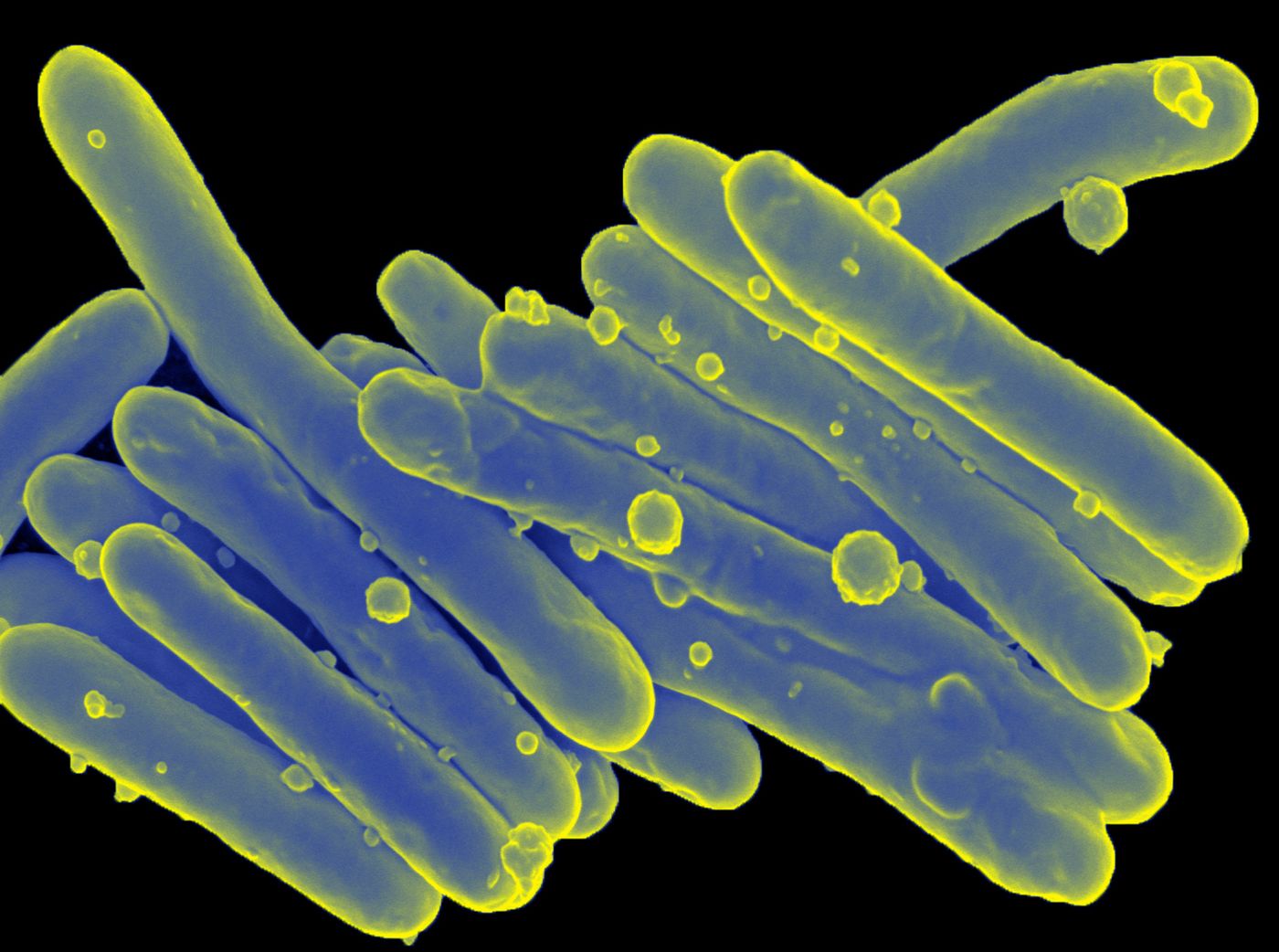
Leprosy, also known as Hansen’s disease, is caused by the bacterium Mycobacterium leprae. These Gram-positive, rod-shaped bacteria depend greatly on their host for survival - they have lost many important metabolic genes through the process of “reductive evolution”. Because of this, they are only able to grow inside host cells. Interestingly, humans and armadillos are the only known, definitive hosts for M. leprae
Inside their hosts, the bacteria live inside of Schwann cells and macrophages. Schwann cells reside in the peripheral nervous system and produce myelin that coats neuronal axons. Once a person is infected, the incubation period can last anywhere from nine months to twenty years! This is because M. leprae replicates extremely slowly - they have a doubling time of 14 days!
As you might expect, M. leprae boasts a number of virulence factors that help it survive inside host cells. First of all, the bacteria keep macrophages from forming phagosomes and lysosomes. Doing so protects the bacteria from being killed by the host. To enter Schwann cells, M. leprae uses a special laminin-binding protein, and a recent study also showed that the bacteria transform these cells into stem cells, a process that helps the bacteria travel throughout the nervous system. When it comes to nutrients, NRAMP proteins help the bacteria transport iron into macrophages - iron is a limiting nutrient for most all bacteria. Finally, M. leprae disrupts the interaction between dendritic cells and T cells, thwarting the immune response - they convince dendritic cells to express PGL-1 on their surface, disrupting their interaction with T cells.
Clinically, leprosy manifests in one of two forms - tuberculoid or lepromatous. In tuberculoid leprosy, the bacteria replicate in Schwann cells and induce a T-cell response. Here, the body does mount an immune response to the bacteria, but nerve damage caused by the infection leads to loss of sensation in the skin. In lepromatous leprosy, the immune response is weak and people develop nodular lesions (containing bacteria) in the skin.
The nerve damage and loss of sensation caused by leprosy make it more likely that people will injure themselves without realizing it. This leads to infections that can cause fingers and toes to be damaged and even die - they don’t “fall off,” contrary to popular belief. Leprosy also causes the body to absorb cartilage, shortening fingers and toes.
How does someone get leprosy? In fact, isn’t it really contagious? You’re most likely to get leprosy when an infected person coughs or sneezes around you. However, if someone is being treated with multi-drug therapy, they are not likely to be contagious. I mentioned that armadillos are another definitive host for M. leprae, but don’t worry, they don’t appear to transmit it to humans.
What about treatment? Leprosy can be treated with a combination of antibiotics and corticosteroids. Drug-resistant strains of bacteria are popping up, so many researchers are working to develop a vaccine. The BCG vaccine for tuberculosis (caused by Mycobacterium tuberculosis, a close relative of M. leprae) has been used with some success to prevent leprosy in both India and Brazil. However, the American Leprosy Missions and the Infectious Disease Research Institute (IDRI) have teamed up to develop a vaccine that consists of four key proteins, and it is currently in clinical trials. The IDRI has also developed a flash-drive-sized diagnostic test for leprosy. If the vaccine is successful, the researchers hope to use the diagnostic test to pinpoint populations most in need of vaccination.
Sources: MicrobeWiki,
American Leprosy Missions,
Cell,
The Guardian,
Public Health,
CDC