Gut Cells and the Immune System Curriculum
The thymus generates a diverse pool of T cells; these cells are essential to the immune response that helps fight infections. T cells are trained in the thymus to recognize foreign invaders as harmful and our cells as “safe.” If T cells begin to recognize our cells as foreign invaders, autoimmune diseases can occur. So, how are these cells trained to distinguish between self and non-self?
Immature T cells populate in the thymus and undergo development to become mature T cells that recognize an antigen. As they develop T cells are trained to recognize an antigen, this antigen is usually derived from a foreign invader but could come from our own cells. Next, T cells can then be tested by cells produced by a gene called AIRE, in the medulla to determine if they interact and recognize “self” antigens. Cells that recognize “self” antigens can be destroyed, while the T cells that recognize “non-self” antigens leave the thymus and travel throughout the body ready to activate the immune response when they recognize a threat.
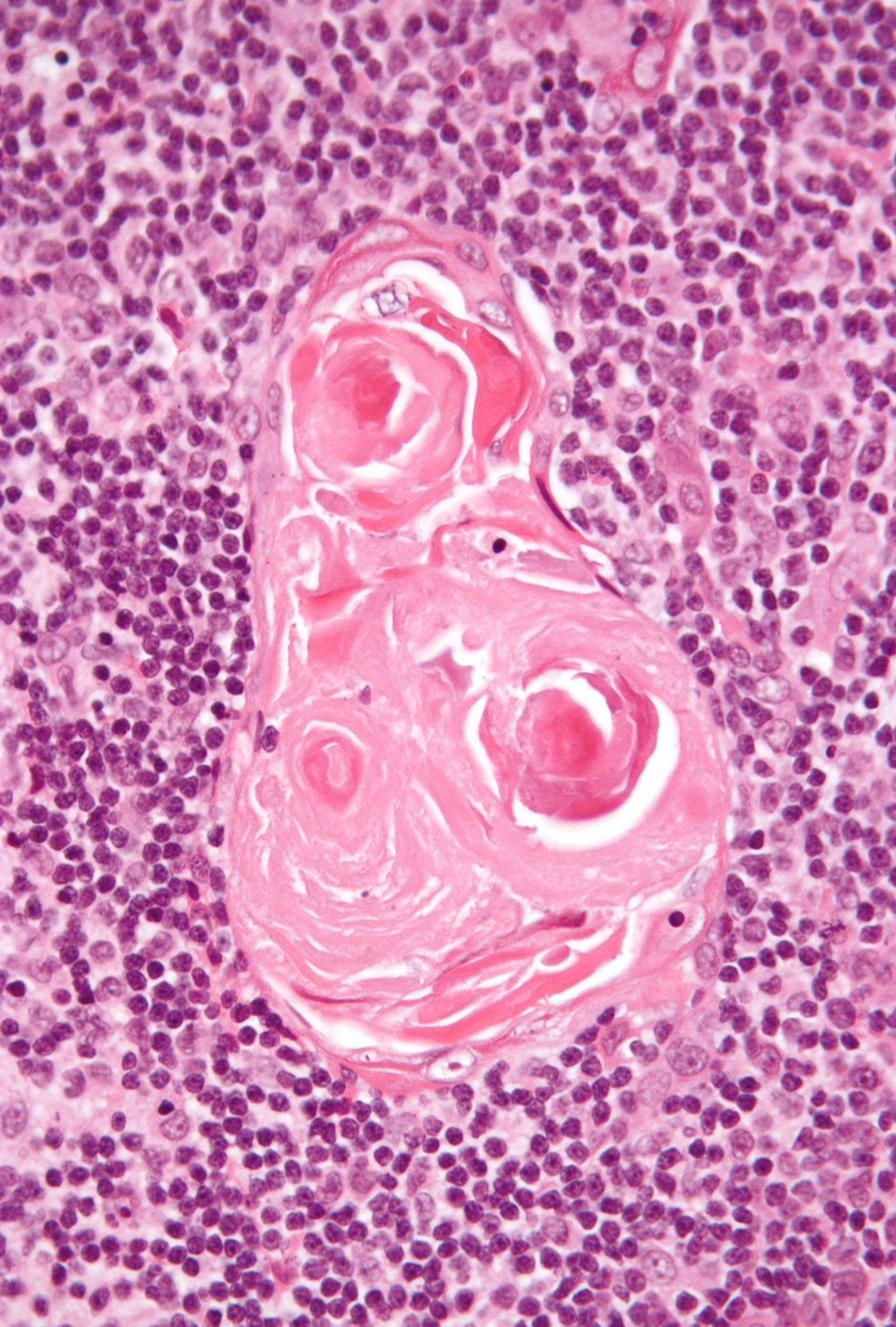
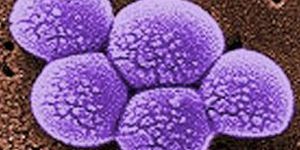
A study published in Nature, from researchers at the University of California San Francisco Diabetes Center, discovered fully formed skin and gut cells in the thymus. In the thymus, there are tiny clusters of cells referred to as Hassall’s corpuscles, the function of which was not known for over 150 years. In particular, this study found that these Hassall’s corpuscles are made up of complex epithelial and sensory cells similar to cells of the skin and gut and surrounded by tuft cells. Tuft cells are a type of sensory cell found in the gut; the cells utilize finger-like protrusions called cilia to “taste” their environment and sample the gut through chemical detectors.
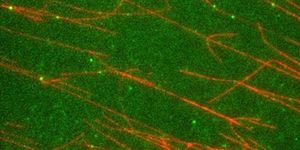
The new study, led by senior author Dr. Mark Anderson, utilized mouse models and showed that these sensory cells played an important role in training the immune system. Researchers traced the development of thousands of AIRE expressing cells and found two subsets that turned off AIRE and began expressing two different genetic programs. These two subsets either differentiated into epithelial cells similar to the skin or started expressing markers similar to tuft cells in the gut. Microscopy showed these two subsets of cells would clump together to form Hassall’s corpuscles. While the tuft cells in the thymus visually appeared similar to the gut, further analysis showed they express different proteins that are necessary to present “self” molecules to T cells. These results indicate a role in the thymus’ immune curriculum.
Researchers wanted to test the importance of these thymic tufts cells by utilizing genetically engineered mice that lacked them. The thymuses of these mice were then transplanted into mice lacking a thymus (naked mice), this allowed for the study of T cell training for the first time without the thymic tuft cells present. Researchers found that without the thymic tuft cells an autoimmune response against the native tuft cells of the naked mice was easily stimulated. “Since the skin and the gut are two of the places where your tissues is directly exposed to the outside world, we hypothesize that Hassall’s corpuscles and the surrounding tuft cells may be the second level of training that essentially simulates these critical environments for maturing T cells to test how they respond,” Anderson said. Having the ability to control the thymus could allow for reprogramming of the immune system in the treatment of various disorders. Therapeutically altering the thymic tuft cells could suppress undesirable immune activity or even lead to the production of designer T cells that attack specific types of cancer. Ongoing work is being done to determine how these thymic tuft cells may be utilized for therapeutic uses.
To read this study click here. For an overview of T cell development watch the video below!